Abstract 摘要
Purpose 目的
Neoadjuvant immunochemotherapy (nICT) for resectable locally advanced esophageal squamous cell carcinoma (LA-ESCC) has attracted widespread attention recently, whose safety and clinical benefit was observed in clinical researches. This study aimed to develop and validate a novel predictor systemic inflammation-tumor markers index (SITI) to predict the pathological complete response (pCR) for resectable LA-ESCC patients receiving nICT.
新辅助免疫化疗(nICT)治疗可切除局部晚期食管鳞状细胞癌(LA-ESCC)近期引发广泛关注,其安全性与临床获益已在临床研究中得到验证。本研究旨在开发并验证一种新型预测指标——全身炎症-肿瘤标志物指数(SITI),用于预测接受 nICT 治疗的可切除 LA-ESCC 患者的病理完全缓解(pCR)。
Patients and Methods 患者与方法
A total of 147 LA-ESCC patients who underwent nICT followed by surgery from February 2020 to April 2022 were included in the study. The dynamic change of inflammatory indexes was compared at baseline, after two cycles of nICT and postoperative one month. Least absolute shrinkage and selection operator (LASSO) regression was performed to avoid collinearity and identify key indexes, with SITI constructed. After univariate and multivariate stepwise forward logistic analyses, a nomogram for pCR prediction was developed.
研究纳入 2020 年 2 月至 2022 年 4 月期间接受新辅助免疫化疗(nICT)后行手术治疗的 147 例局部晚期食管鳞癌(LA-ESCC)患者。比较基线水平、完成两个周期 nICT 后及术后 1 个月炎症指标的动态变化。采用最小绝对收缩与选择算子(LASSO)回归消除共线性并筛选关键指标,构建系统性炎症-肿瘤指数(SITI)。通过单因素及多因素逐步向前 Logistic 回归分析,最终建立预测病理完全缓解(pCR)的列线图模型。
Results 结果
41(27.9%) patients achieved pCR among 147 resectable LA-ESCC patients received nICT. Compared with baseline, most inflammatory indexes were significantly decreased at postoperative one month. 5 key indexes were identified and then a predictive index named SITI was constructed. The result showed that lower SITI and earlier clinical tumor node metastasis (cTNM) stage were more likely to achieve pCR. The nomogram for pCR prediction had excellent discrimination performance (C-index = 0.791).
在 147 例接受新辅助免疫化疗(nICT)的可切除局部晚期食管鳞癌(LA-ESCC)患者中,41 例(27.9%)达到病理完全缓解(pCR)。与基线相比,术后 1 个月多数炎症指标显著下降。研究筛选出 5 个关键指标并构建了名为 SITI 的预测指数,结果显示较低的 SITI 值和更早的临床肿瘤淋巴结转移(cTNM)分期更易获得 pCR。用于预测 pCR 的列线图模型具有优异的区分效能(C 指数=0.791)。
Conclusion 结论
The SITI is an independent predictor for pCR in resectable LA-ESCC patients received nICT. To our knowledge, our nomogram is the first model using systemic inflammation-tumor markers for pCR prediction and may be a promising predictor to effectively differentiate pCR for nICT in LA-ESCC patients.
SITI 是接受 nICT 治疗的可切除 LA-ESCC 患者获得 pCR 的独立预测因子。据我们所知,本列线图是首个应用全身炎症-肿瘤标志物预测 pCR 的模型,可能成为有效区分 LA-ESCC 患者 nICT 后 pCR 的潜在预测工具。
Keywords: esophageal squamous cell carcinoma, neoadjuvant therapy, immunotherapy, pathologic complete response, inflammation, nomogram
关键词:食管鳞状细胞癌、新辅助治疗、免疫治疗、病理完全缓解、炎症、列线图
Introduction 引言
Esophageal cancer is a global health challenge with high cancer incidence and cancer-related death worldwide.1,2 The majority of esophageal cancer cases are found in Asia, with 49% in China. Esophageal squamous cell carcinoma (ESCC) is the most common pathological type in China.3,4 Neoadjuvant chemotherapy (nCT) or chemoradiotherapy (nCRT) plus surgery has become the preferred treatment for locally advanced esophageal squamous cell carcinoma (LA-ESCC), although the long-time survival for which is still unsatisfactory.5–8
食管癌是全球范围内癌症发病率和癌症相关死亡率均较高的健康挑战。 1 2 大多数食管癌病例分布在亚洲,其中中国占 49%。食管鳞状细胞癌(ESCC)是我国最常见的病理类型。 3 4 新辅助化疗(nCT)或放化疗(nCRT)联合手术已成为局部晚期食管鳞状细胞癌(LA-ESCC)的首选治疗方案,但其远期生存仍不理想。 5–8
Recently, immunotherapy combined with chemotherapy has become the new standard of first-line treatment for advanced ESCC,9–13 which has brought widespread attention to attempts at neoadjuvant immunochemotherapy (nICT) for resectable LA-ESCC. At present, nICT is recommended for patients with LA-ESCC in clinical studies, and its safety and clinical benefit was observed.14–17 Pathological complete response (pCR) is considered to be an important therapeutic effect of neoadjuvant therapy and a good surrogate marker of postoperative survival. However, studies regarding reliable pCR prediction in resectable LA-ESCC patients receiving nICT are lacking. Although the expression of programmed cell death ligand-1 (PD-L1), tumor mutation load, microsatellite stability, and T cell function have been reported to be associated with immunotherapy efficacy,18,19 these tests remain difficult for some patients due to medical conditions and economic constraints. Therefore, it is of great significance to find more affordable, effective and accurate indicators and establish more practical predictive models for personalized pCR prediction for patients with LA-ESCC.
近年来,免疫治疗联合化疗已成为晚期 ESCC 一线治疗的新标准, 9–13 这使得可切除 LA-ESCC 的新辅助免疫化疗(nICT)尝试受到广泛关注。目前临床研究推荐 LA-ESCC 患者接受 nICT 治疗,并观察到其安全性和临床获益。 14–17 病理完全缓解(pCR)被认为是新辅助治疗的重要疗效指标和术后生存的良好替代标志物。然而,针对接受 nICT 治疗的可切除 LA-ESCC 患者可靠 pCR 预测的研究仍较缺乏。尽管程序性死亡配体-1(PD-L1)表达、肿瘤突变负荷、微卫星稳定性及 T 细胞功能已被报道与免疫治疗疗效相关, 18 19 但由于医疗条件和经济因素限制,这些检测对部分患者而言仍难以实施。因此,寻找更经济有效、精准的指标并建立更具实践价值的预测模型用于 LA-ESCC 患者个体化 pCR 预测具有重要意义。
Several inflammatory indexes have been reported to be associated with pCR and prognosis after neoadjuvant therapy for esophageal cancer, such as lymphocyte (LY),20,21 neutrophil to lymphocyte ratio (NLR),21,22 platelet to lymphocyte ratio (PLR),21,23 lymphocyte to monocyte ratio (LMR),24 and systemic immune inflammation index (SII).23 In this study, we explored the dynamics of inflammatory indexes at baseline, after two cycles of nICT and postoperative one month. Based on LASSO regression analysis, 5 key markers were identified, including CA125, CEA and neutrophil (NEUT) before nICT, monocyte (MONO) and LMR after nICT. Then we developed a novel predictor named systemic inflammation-tumor markers index (SITI) for pCR. Finally, SITI and clinical tumor node metastasis (cTNM) stage were identified as the independent significant predictors for pCR and used to develop a novel nomogram to accurately and effectively differentiate pCR for nICT in resectable LA-ESCC patients.
已有研究报道多种炎症指标与食管癌新辅助治疗后病理完全缓解(pCR)及预后相关,如淋巴细胞(LY)、 20 21 中性粒细胞与淋巴细胞比值(NLR)、 21 22 血小板与淋巴细胞比值(PLR)、 21 23 淋巴细胞与单核细胞比值(LMR)、 24 以及全身免疫炎症指数(SII)等。 23 本研究探索了基线期、两个周期新辅助免疫化疗后及术后 1 个月炎症指标的动态变化。通过 LASSO 回归分析筛选出 5 个关键标志物,包括新辅助免疫化疗前 CA125、CEA 及中性粒细胞(NEUT),新辅助免疫化疗后单核细胞(MONO)及 LMR,并构建新型预测指标——全身炎症-肿瘤标志物指数(SITI)用于预测 pCR。最终确定 SITI 和临床肿瘤淋巴结转移(cTNM)分期为 pCR 的独立显著预测因子,并基于此开发新型列线图模型,可精准有效区分可切除局部晚期食管鳞癌患者接受新辅助免疫化疗后的病理完全缓解状态。
Materials and Methods 材料与方法
Patients 患者
In this retrospective single-center study, we collected data from 168 patients with esophageal cancer who underwent nICT followed by surgery at the First Affiliated Hospital of Zhengzhou University from February 2020 to April 2022. The inclusion criteria were as follows: (1) diagnosis of ESCC based on preoperative pathological examination; (2) ESCC confirmed with clinical stage II–IVA based on computed tomography (CT) and endoscopic ultrasonography (EUS); (3) Surgery after nICT, with R0 resection; (4) age ≤80 years, with a good general condition and normal cardiopulmonary and other organ function; and (5) well-documented medical records and follow-up. The exclusion criteria were as follows: (1) infection, autoimmune disease or hematologic disease; (2) other synchronous or previous malignancy; and (3) immunotherapy could not be administered due to a serious adverse event. We excluded 6 patients who received nICT in combination with radiotherapy or targeted therapy. In addition, only 7 patients received 1 cycle, 5 patients received 3 cycles, and 3 patients received 4 cycles of nICT. We ended up enrolling 147 patients in this study.
在这项回顾性单中心研究中,我们收集了 2020 年 2 月至 2022 年 4 月在郑州大学第一附属医院接受新辅助免疫化疗(nICT)后行手术治疗的 168 例食管癌患者数据。纳入标准如下:(1)术前病理检查诊断为食管鳞状细胞癌(ESCC);(2)经计算机断层扫描(CT)和内镜超声(EUS)确诊为临床 II-IVA 期 ESCC;(3)nICT 后行手术治疗且达到 R0 切除;(4)年龄≤80 岁,一般状况良好且心肺等器官功能正常;(5)病历资料及随访记录完整。排除标准包括:(1)存在感染、自身免疫性疾病或血液系统疾病;(2)合并其他同步或既往恶性肿瘤;(3)因严重不良事件无法完成免疫治疗。我们排除了 6 例联合放疗或靶向治疗的 nICT 患者。此外,仅 7 例患者接受 1 个周期、5 例接受 3 个周期、3 例接受 4 个周期的 nICT 治疗。最终本研究共纳入 147 例患者。
Treatment 治疗
Patients received neoadjuvant chemotherapy combined with immunotherapy every 3 weeks. Neoadjuvant chemotherapy has two regimens: (1) docetaxel plus nedaplatin; (2) paclitaxel plus cisplatin or nedaplatin. Immunotherapy (pembrolizumab, camrelizumab, tislelizumab or sintilimab 200 mg) was performed on day 1 of each cycle. After 2 cycles of nICT, the laparo-thoracoscopic McKeown surgery was performed. Pathological examination of the surgically removed tissue specimens was performed, and the tumor and lymph nodes were independently evaluated by two pathologists from our hospital after neoadjuvant treatment. The histological type of esophageal cancer was determined according to the 2019 edition of the World Health Organization (WHO) Classification of Tumors of the Digestive System. The tumor regression grade (TRG) was based on the criteria of the College of American Pathologists (CAP), which is in line with the approach recommended by the National Comprehensive Cancer Network (NCCN) guidelines for the management of esophageal cancer.4 The TNM stage was determined according to the International Union Against Cancer (UICC)/American Joint Committee on Cancer (AJCC) TNM Staging System (8th edition, 2017).25
患者每 3 周接受一次新辅助化疗联合免疫治疗。新辅助化疗有两种方案:(1)多西他赛联合奈达铂;(2)紫杉醇联合顺铂或奈达铂。免疫治疗(帕博利珠单抗、卡瑞利珠单抗、替雷利珠单抗或信迪利单抗 200 mg)在每个周期第 1 天进行。完成 2 周期新辅助治疗后,行腹腔镜-胸腔镜 McKeown 手术。对手术切除的组织标本进行病理学检查,新辅助治疗后肿瘤及淋巴结由我院两名病理医师独立评估。食管癌组织学类型依据 2019 年版世界卫生组织(WHO)《消化系统肿瘤分类》确定。肿瘤退缩分级(TRG)采用美国病理学家协会(CAP)标准,该标准与国立综合癌症网络(NCCN)食管癌管理指南推荐方案一致。 4 TNM 分期根据国际抗癌联盟(UICC)/美国癌症联合委员会(AJCC)TNM 分期系统(第 8 版,2017)确定。 25
Outcomes and Follow Up
结果与随访
The primary clinical endpoint was the pathological response of the primary tumor. Patients without residual tumor cells of the resected tumor specimen and lymph node metastasis (ypT0N0) were considered to have achieved pCR. After treatment, patients were regularly checked, including physical examinations, tumor markers tests and contrast CT examinations. The last follow-up time was completed in October 2022.
主要临床终点是原发肿瘤的病理反应。切除肿瘤标本及淋巴结转移灶中无残留肿瘤细胞(ypT0N0)的患者被认为达到 pCR。治疗后对患者进行定期复查,包括体格检查、肿瘤标志物检测和增强 CT 检查。末次随访时间截至 2022 年 10 月。
Clinical Features and Inflammatory Indexes
临床特征与炎症指标
The data of clinical characteristics, clinical staging and hematological indexes, were retrospectively collected and arranged. Hematological indicators of patients extracted from the medical record system included NEUT, LY, MONO, NLR, PLR, LMR, AISI, and SII before nICT treatment, after 2 cycles of nICT treatment, and 1 month after surgery. The 4 hematological indexes, including platelet (PLT), NEUT, LY and MONO, were obtained before nICT, after 2 cycles of nICT and postoperative one month. The NLR, PLR and LMR were defined as NEUTs divided by LYs, PLTs divided by LYs and LYs divided by MONOs, respectively. According to previously published study, variables were calculated by the following formula: aggregate index of systemic inflammation (AISI) = MONO × PLT× NEUT/LY,26 SII = PLT × NEUT/LY.27
回顾性收集并整理患者的临床特征、临床分期及血液学指标数据。从病历系统中提取的血液学指标包括 nICT 治疗前、nICT 治疗 2 周期后及术后 1 个月的中性粒细胞(NEUT)、淋巴细胞(LY)、单核细胞(MONO)、中性粒细胞-淋巴细胞比值(NLR)、血小板-淋巴细胞比值(PLR)、淋巴细胞-单核细胞比值(LMR)、全身炎症综合指数(AISI)及全身免疫炎症指数(SII)。血小板(PLT)、NEUT、LY、MONO 这 4 项血液学指标分别于 nICT 治疗前、nICT 治疗 2 周期后及术后 1 个月获取。NLR、PLR 及 LMR 分别定义为 NEUT 计数除以 LY 计数、PLT 计数除以 LY 计数以及 LY 计数除以 MONO 计数。参照既往研究,按以下公式计算变量:全身炎症综合指数(AISI)= MONO × PLT × NEUT/LY, 26 全身免疫炎症指数(SII)= PLT × NEUT/LY。 27
Statistical Analysis 统计分析
R software (version 4.2.0) and IBM SPSS 26.0 were carried out to conduct all statistical analyses. Continuous variables were performed by t-tests and categorical variables were analyzed by Chi-square or Fisher’s exact tests. Based on the ratio of hematological markers before and after nICT, the least absolute shrinkage and selection operator (LASSO) regression was performed to avoid collinearity by using the “glmnet” package in R. The receiver operating characteristic curve (ROC) analysis was performed to group 147 patients by the best cutoff value and patients was divided into high and low groups.28 Univariate logistic analysis was performed to determine whether the indicator is positive or negative. The high indicator group of adverse factors is defined as a risk score of 1, and the high indicator group of favorable factors is defined as a score of 0. We calculated the cumulative score of difficulty to achieve pCR, and the formula is as follows: Cumulative Score = pre-NEUT Score (0/1) + pre-CA125 Score (0/1) + pre-CEA Score (0/1) + post-MONO Score (0/1) + post-LMR Score (0/1). Referring to the predictive ability of cumulative scores on pCR, patients with cumulative scores of 0–1, 2, and 3–5 were then defined as the three grades of SITI. Univariate and multivariate stepwise forward logistic regression analyses were used to identify the predictors of pCR, with the odds ratios (ORs) and 95% confidence intervals (CIs) calculated. Then, independent predictive factors of pCR prediction were selected to establish and validate a nomogram. The calibration curve, ROC curve, decision curve analyses (DCA) and clinical impact curve were used to assess the discriminative ability of pCR prediction. All probabilities were two-tailed, and the level of significance was set at 0.05.
采用 R 软件(4.2.0 版本)和 IBM SPSS 26.0 进行所有统计分析。连续变量采用 t 检验,分类变量采用卡方检验或 Fisher 精确检验分析。基于新辅助免疫化疗(nICT)前后血液学标志物比值,使用 R 软件"glmnet"包进行最小绝对值收缩和选择算子(LASSO)回归以避免共线性。通过受试者工作特征曲线(ROC)分析确定最佳截断值对 147 例患者进行分组,将患者分为高组和低组。 28 采用单因素 logistic 分析判定指标的正负性。将不良因素的高指标组定义为风险评分为 1,有利因素的高指标组定义为评分为 0。我们计算了实现病理完全缓解(pCR)困难程度的累积评分,公式如下:累积评分=新辅助免疫化疗前中性粒细胞评分(0/1)+新辅助免疫化疗前 CA125 评分(0/1)+新辅助免疫化疗前 CEA 评分(0/1)+新辅助免疫化疗后单核细胞评分(0/1)+新辅助免疫化疗后淋巴细胞-单核细胞比值(LMR)评分(0/1)。 参考累积评分对 pCR 的预测能力,将累积评分为 0–1 分、2 分和 3–5 分的患者分别定义为 SITI 的三个分级。采用单因素和多因素逐步向前 Logistic 回归分析确定 pCR 的预测因子,并计算比值比(OR)及 95%置信区间(CI)。随后,筛选 pCR 预测的独立预测因素以构建并验证列线图模型。通过校准曲线、ROC 曲线、决策曲线分析(DCA)及临床影响曲线评估该模型对 pCR 的判别效能。所有概率均为双尾检验,显著性水平设定为 0.05。
Results 结果
Patient Characteristics 患者特征
Ultimately, there were 147 patients with LA-ESCC who underwent nICT followed by radical resection in this study (Figure 1). The study enrolled 105 (71.4%) men and 42 (28.6%) women with a mean age of 63.4 ± 7.0 years. Most patients were diagnosed at the stage of cT3 (47.6%), cN0 (59.2%), and cTNM II (55.1%), respectively. Among the patients, 41 (27.9%) cases achieved pCR. The detailed baseline clinical characteristics of the patients are summarized in Table 1.
本研究最终纳入 147 例接受新辅助免疫化疗(nICT)后行根治性切除术的局部晚期食管鳞癌(LA-ESCC)患者( Figure 1 )。其中男性 105 例(71.4%),女性 42 例(28.6%),平均年龄 63.4±7.0 岁。多数患者临床分期为 cT3(47.6%)、cN0(59.2%)和 cTNM II 期(55.1%)。41 例(27.9%)患者达到病理完全缓解(pCR)。患者基线临床特征详见 Table 1 。
Figure 1. 图 1.
The flow diagram of selection of eligible LA-ESCC patients who received nICT plus radical resection.
接受 nICT 联合根治性切除术的符合条件 LA-ESCC 患者筛选流程图。
Table 1. 表 1.
Characteristics for 147 LA-ESCC Patients
147 例 LA-ESCC 患者的特征
| Parameter 参数 | Value (n=147) 数值 (n=147) |
|---|---|
| Age (years) 年龄(岁) | |
| ≤64.5 | 72 (49.0%) |
| >64.5 | 75 (51.0%) |
| Sex: 性别: | |
| Female 女性 | 42 (28.6%) |
| Male 男 | 105 (71.4%) |
| Smoking history: 吸烟史: | |
| No 无 | 125 (85.0%) |
| Yes 是 | 22 (15.0%) |
| Drinking history: 饮酒史: | |
| No | 117 (79.6%) |
| Yes 是 | 30 (20.4%) |
| Hypertension history: 高血压病史: | |
| No 否 | 105 (71.4%) |
| Yes 是 | 42 (28.6%) |
| Diabetes history: 糖尿病病史: | |
| No 不 | 138 (93.9%) |
| Yes 是 | 9 (6.1%) |
| CHD history: CHD 病史: | |
| No 不 | 139 (94.6%) |
| Yes 是 | 8 (5.4%) |
| Location: 位置: | |
| Upper 上 | 21 (14.3%) |
| Middle 中间 | 75 (51.0%) |
| Lower 下部 | 51 (34.7%) |
| cT stage: cT 分期: | |
| T2 | 56 (38.1%) |
| T3 | 70 (47.6%) |
| T4 | 21 (14.3%) |
| cN stage: cN 分期: | |
| N0 | 87 (59.2%) |
| N1 | 60 (40.8%) |
| cTNM stage: cTNM 分期: | |
| II | 81 (55.1%) |
| III | 38 (25.9%) |
| IVA | 28 (19.0%) |
| Differentiation: 分化: | |
| Well 好 | 14 (9.5%) |
| Moderate 中度 | 105 (71.4%) |
| Poor 差 | 28 (19.1%) |
| pCR: | |
| No 否 | 106 (72.1%) |
| Yes 是 | 41 (27.9%) |
| Immunotherapy: 免疫治疗: | |
| Camrelizumab 卡瑞利珠单抗 | 131 (89.1%) |
| Sintilimab | 6 (4.1%) |
| Pembrolizumab 帕博利珠单抗 | 5 (3.4%) |
| Tislelizumab 替雷利珠单抗 | 3 (2.0%) |
| Toripalimab 特瑞普利单抗 | 2 (1.4%) |
| CA125 (U/mL) | 9.72 ± 4.46 |
| CA199 (U/mL) | 12.80 ± 14.70 |
| CEA (U/mL) CEA(U/mL) | 2.72 ± 4.97 |
Abbreviations: LA-ESCC, locally advanced esophageal squamous cell carcinoma; CHD, coronary heart disease; TNM, tumor node metastasis; pCR, pathological complete response; CA, carbohydrate antigen; CEA, Carcinoembryonic antigen.
缩写:LA-ESCC,局部进展期食管鳞状细胞癌;CHD,冠心病;TNM,肿瘤淋巴结转移分期;pCR,病理学完全缓解;CA,糖类抗原;CEA,癌胚抗原。
Inflammatory and Nutritional Indexes Grouped by pCR
按 pCR 分组的炎症与营养指标
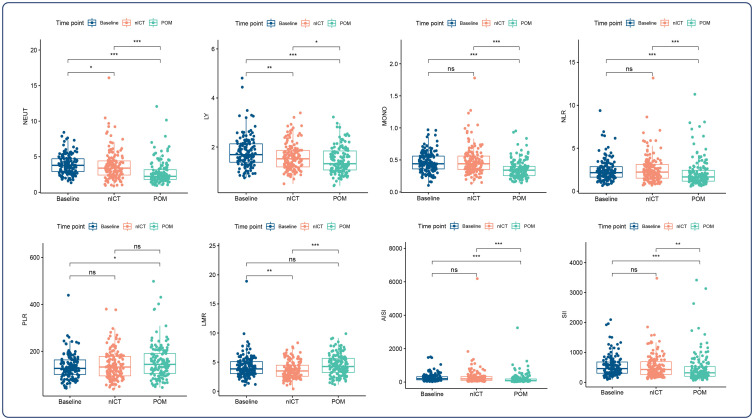
Figure 2 illustrates dynamic changes in inflammatory indexes during baseline, after two cycles of nICT, and postoperative one month for 147 LA-ESCC patients. Compared with baseline, most indicators except for PLR were significantly decreased at postoperative one month, while only NEUT, LY and LMR were significantly decreased after nICT. Consistent results were also observed in 41 patients with pCR in Supplemental Figure 1. Further, these inflammatory indicators were assessed based on pCR, respectively (Table 2). There were no statistically significant differences in all indexes at baseline and postoperative one month between two groups. Interestingly, the pCR group had a higher MONO and lower LMR than the non-pCR group after nICT treatment.
Figure 2 展示了 147 例 LA-ESCC 患者基线期、新辅助免疫化疗(nICT)两周期后及术后 1 个月炎症指标动态变化。与基线期相比,除 PLR 外多数指标术后 1 个月均显著降低,而 nICT 后仅 NEUT、LY 及 LMR 显著降低。在 Supplemental Figure 1 的 41 例 pCR 患者中也观察到一致结果。进一步基于 pCR 状态分别评估这些炎症指标( Table 2 )。两组基线期及术后 1 个月所有指标均无统计学差异。值得注意的是,nICT 治疗后 pCR 组较非 pCR 组具有更高的 MONO 及更低的 LMR。
Figure 2. 图 2.
Dynamic changes of inflammatory indexes in 147 LA-ESCC patients at baseline, after 2 cycles of nICT and postoperative one month. ns showed no statistical difference; *P<0.05, **P<0.01, ***P<0.001.
147 例 LA-ESCC 患者基线期、接受 2 个周期 nICT 后及术后一个月炎症指标的动态变化。ns 表示无统计学差异;*P<0.05,**P<0.01,***P<0.001。
Table 2. 表 2.
Inflammatory and Nutritional Scores at Different Time Points
不同时间点的炎症和营养评分
| pCR (n = 41) pCR(n = 41) |
Non-pCR (n = 106) 非 pCR(n = 106) |
P | |
|---|---|---|---|
| Baseline 基线 | |||
| NEUT (10^9/L) NEUT(10^9/L) | 4.20 ± 1.33 | 3.82 ± 1.37 | 0.130 |
| LY (10^9/L) LY (10^9/升) | 1.79 ± 0.54 | 1.81 ± 0.68 | 0.800 |
| MONO (10^9/L) | 0.49 ± 0.14 | 0.46 ± 0.17 | 0.181 |
| NLR | 2.60 ± 1.48 | 2.36 ± 1.21 | 0.359 |
| PLR | 135 ± 45.60 | 134 ± 55.20 | 0.946 |
| LMR | 3.82 ± 1.35 | 4.38 ± 2.13 | 0.059 |
| AISI | 303 ± 244 | 263 ± 249 | 0.374 |
| SII | 598 ± 390 | 530 ± 337 | 0.334 |
| nICT | |||
| NEUT (10^9/L) | 4.18 ± 1.91 | 3.62 ± 2.14 | 0.126 |
| LY (10^9/L) | 1.64 ± 0.59 | 1.58 ± 0.53 | 0.556 |
| MONO (10^9/L) | 0.55 ± 0.21 | 0.46 ± 0.23 | 0.023 |
| NLR | 2.84 ± 1.72 | 2.46 ± 1.59 | 0.226 |
| PLR | 150 ± 65.20 | 139 ± 59.10 | 0.355 |
| LMR | 3.19 ± 1.22 | 3.88 ± 1.53 | 0.005 |
| AISI | 337 ± 227 | 305 ± 647 | 0.657 |
| SII | 596 ± 322 | 516 ± 449 | 0.233 |
| POM | |||
| NEUT (10^9/L) | 2.71 ± 1.32 | 2.78 ± 1.79 | 0.782 |
| LY (10^9/L) | 1.54 ± 0.60 | 1.44 ± 0.50 | 0.322 |
| MONO (10^9/L) | 0.36 ± 0.15 | 0.36 ± 0.14 | 0.888 |
| NLR | 2.02 ± 1.34 | 2.19 ± 1.73 | 0.532 |
| PLR | 144 ± 53.80 | 160 ± 79.20 | 0.155 |
| LMR | 4.63 ± 1.78 | 4.44 ± 1.82 | 0.582 |
| AISI | 169 ± 178 | 212 ± 371 | 0.352 |
| SII | 417 ± 309 | 492 ± 554 | 0.300 |
Abbreviations: pCR, pathological complete response; nICT, neoadjuvant immunochemotherapy; POM, postoperative one month; NEUT, neutrophil; LY, lymphocyte; MONO, monocyte; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; LMR, lymphocyte to monocyte ratio; AISI, aggregate index of systemic inflammation; SII, systemic immune-inflammation index.
缩写:pCR,病理完全缓解;nICT,新辅助免疫化疗;POM,术后一个月;NEUT,中性粒细胞;LY,淋巴细胞;MONO,单核细胞;NLR,中性粒细胞与淋巴细胞比值;PLR,血小板与淋巴细胞比值;LMR,淋巴细胞与单核细胞比值;AISI,全身炎症综合指数;SII,全身免疫炎症指数。
Identification of Key Indexes and Establishment of a Classifier
关键指标识别与分类器建立
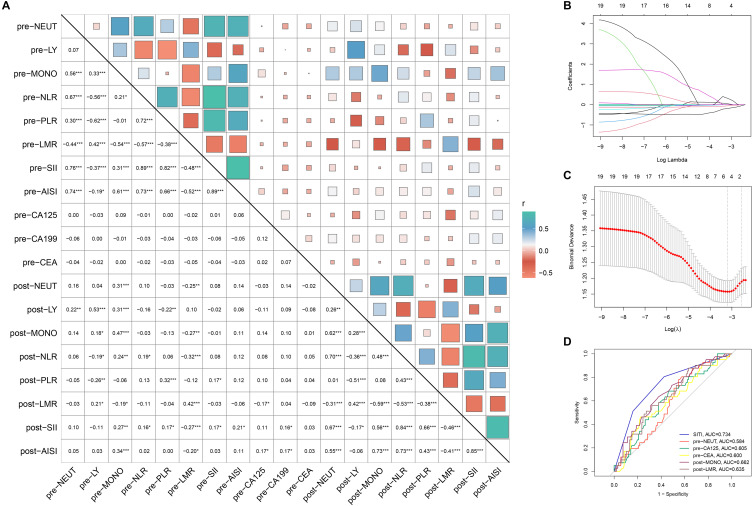
In Figure 3, a correlation heatmap is shown for 8 inflammatory indexes before and after nICT and tumor markers at baseline in 147 LA-ESCC patients. In order to avoid collinearity, LASSO regression was performed and 5 key markers were identified (Figure 3A–C). The ROC analysis indicated that the optimal cutoff value for CA125, CEA, pre-NEUT, post-MONO and post-LMR was 8.90 U/mL, 1.11 U/mL, 3.44*10^9/L, 0.455*10^9/L and 4.194 (Table 3), and the area under the curve (AUC) was 0.605, 0.600, 0.584, 0.662 and 0.635 (Figure 3D), respectively. Then 147 patients were divided into high and low groups based on the cutoff value for ROC analysis. And finally a scoring system was developed, with a larger AUC (0.734) for pCR (Figure 3D). Thus, the patients were divided into three groups based on the SITI for further analysis. Table 4 revealed that baseline clinical characteristics grouped by SITI were significantly associated with pCR (P < 0.001).
Figure 3 显示了 147 例局部晚期食管鳞癌(LA-ESCC)患者新辅助免疫化疗(nICT)前后 8 项炎症指标与基线肿瘤标志物的相关性热图。为避免共线性,采用 LASSO 回归筛选出 5 个关键标志物( Figure 3A–C )。ROC 分析提示 CA125、CEA、治疗前中性粒细胞(pre-NEUT)、治疗后单核细胞(post-MONO)和治疗后淋巴细胞-单核细胞比值(post-LMR)的最佳截断值分别为 8.90 U/mL、1.11 U/mL、3.44×10^9/L、0.455×10^9/L 和 4.194( Table 3 ),其曲线下面积(AUC)分别为 0.605、0.600、0.584、0.662 和 0.635( Figure 3D )。根据截断值将患者分为高、低危组进行 ROC 分析,最终建立的评分系统对病理完全缓解(pCR)具有更高 AUC(0.734)( Figure 3D )。基于 SITI 评分将患者分为三组, Table 4 显示 SITI 分组的基线临床特征与 pCR 显著相关(P<0.001)。
Figure 3. 图 3.
Identification of key indexes and construction of SITI by LASSO logistic regression. (A) A correlation matrix is represented regarding 19 indicators. (B) LASSO coefficient profiles of the 19 indicators. (C) Ten-fold cross-validation for tuning parameter selection. (D) ROC for SITI and its constituent indicators. *P<0.05, **P<0.01, ***P<0.001.
关键指标的识别及通过 LASSO 逻辑回归构建 SITI。(A) 19 项指标的相关性矩阵。(B) 19 项指标的 LASSO 系数轨迹图。(C) 十折交叉验证用于调整参数选择。(D) SITI 及其组成指标的 ROC 曲线。*P<0.05,**P<0.01,***P<0.001。
Table 3. 表 3.
Cut off Value Based on ROC Analysis and Scoring System Constructed
基于 ROC 分析的截断值及构建的评分系统
| Cut off Value 临界值 | Univariate OR (>Cut off Value vs ≤Cut off Value, 97.5% CI) 单因素 OR(>截断值 vs ≤截断值,97.5% CI) |
P value P 值 | Score (>Cut off Value) 评分 (>临界值) |
Score (≤Cut off Value) 评分(≤截断值) |
|
|---|---|---|---|---|---|
| pre-NEUT | 3.44*10^9/L 3.44×10^9/L | 2.943 (1.323, 7.102) | 0.0111 | 0 | 1 |
| pre-CA125 | 8.90 U/mL 8.90 单位/毫升 | 0.399 (0.182, 0.840) | 0.0179 | 1 | 0 |
| pre-CEA | 1.11 U/mL 1.11 单位/毫升 | 0.339 (0.157, 0.727) | 0.0055 | 1 | 0 |
| post-MONO MONO 后 | 0.455*10^9/L | 2.860 (1.370, 6.151) | 0.0058 | 0 | 1 |
| post-LMR | 4.194 | 0.239 (0.077, 0.611) | 0.0057 | 1 | 0 |
Abbreviations: pre-NEUT, neutrophil at baseline; pre-CA125, carbohydrate antigen 125 at baseline; pre-CEA, Carcinoembryonic antigen at baseline; post-MONO, monocyte after nICT; post-LMR, lymphocyte to monocyte ratio after nICT; OR, odds ratio; CI, confidence interval.
缩写:pre-NEUT,基线中性粒细胞;pre-CA125,基线糖类抗原 125;pre-CEA,基线癌胚抗原;post-MONO,新辅助免疫治疗后单核细胞;post-LMR,新辅助免疫治疗后淋巴细胞与单核细胞比值;OR,比值比;CI,置信区间。
Table 4. 表 4.
The Clinical Characteristics Grouped by SITI
按 SITI 分组的临床特征
| Parameter 参数 | SITI 1 (n = 38) | SITI 2 (n = 40) | SITI 3 (n = 69) | P value P 值 |
|---|---|---|---|---|
| Age (years, ≤64.5/>64.5) 年龄(岁,≤64.5/>64.5) |
16/22 | 18/22 | 38/31 | 0.368 |
| Sex (Female/Male) 性别(女/男) | 8/30 | 9/31 | 25/44 | 0.153 |
| Smoking history (Yes/No) 吸烟史(Yes/No) |
4/34 | 7/33 | 11/58 | 0.656 |
| Drinking history (Yes/No) 饮酒史 (Yes/No) |
6/32 | 14/26 | 10/59 | 0.027 |
| Hypertension history (Yes/No) 高血压病史 (Yes/No) |
11/27 | 13/27 | 18/51 | 0.773 |
| Diabetes history (Yes/No) 糖尿病病史 (Yes/No) |
2/36 | 5/35 | 2/67 | 0.175 |
| CHD history (Yes/No) CHD 病史(是/否) | 4/34 | 0/40 | 4/65 | 0.122 |
| Location (Upper/Middle/Lower) 位置 (上部/中部/下部) |
7/13/18 | 3/26/11 | 11/36/22 | 0.090 |
| cT Stage (2/3/4) cT 分期(2/3/4) | 15/18/5 | 12/22/6 | 29/30/10 | 0.783 |
| cN Stage (0/+) cN 分期(0/+) | 26/12 | 23/17 | 38/31 | 0.392 |
| cTNM Stage (II/III/IVA) cTNM 分期(II/III/IVA) | 25/6/7 | 21/11/8 | 35/21/13 | 0.526 |
| Differentiation (High/Medium/Low) 分化(高/中/低) |
4/24/10 | 5/28/7 | 5/53/11 | 0.553 |
| pCR (Yes/No) pCR(是/否) | 21/17 | 12/28 | 8/61 | <0.001 |
Abbreviations: SITI, systemic inflammation-tumor markers index; CHD, coronary heart disease; pCR, pathological complete response.
缩写:SITI,systemic inflammation-tumor markers index;CHD,coronary heart disease;pCR,pathological complete response。
Evaluation of the SITI as an Independent Factor
SITI 作为独立因素的评估
To determine independent predicted factors for pCR, univariate and multivariate logistic regression analyses were performed for 147 LA-ESCC patients among the SITI and other clinical characteristics. Table 5 shows that predictive factors associated with pCR in univariate logistic regression included cN Stage, cTNM and the SITI. According to the multivariate stepwise forward logistic regression analyses, the results indicated that the SITI remained an independent predictor of pCR in resectable LA-ESCC patients treated with nICT (2 vs 1: OR=0.361, 95% CI = 0.134–0.968, P = 0.0437; 3 vs 1: OR=0.104, 95% CI=0.038–0.290, P < 0.0001). Besides, cTNM was also an independent predictor of pCR (III vs II: OR=0.330, 95% CI=0.115–0.942, P = 0.0388; IVA vs II: OR=0.158, 95% CI = 0.041–0.614, P = 0.0076).
为确定 pCR 的独立预测因素,我们对 147 例 LA-ESCC 患者的 SITI 及其他临床特征进行了单因素和多因素 logistic 回归分析。 Table 5 显示单因素 logistic 回归中与 pCR 相关的预测因素包括 cN 分期、cTNM 分期及 SITI。通过多因素逐步前向 logistic 回归分析,结果表明在 nICT 治疗的可切除 LA-ESCC 患者中,SITI 仍是 pCR 的独立预测因子(2 vs 1:OR=0.361,95% CI=0.134–0.968,P=0.0437;3 vs 1:OR=0.104,95% CI=0.038–0.290,P<0.0001)。此外,cTNM 分期也是 pCR 的独立预测因子(III vs II:OR=0.330,95% CI=0.115–0.942,P=0.0388;IVA vs II:OR=0.158,95% CI=0.041–0.614,P=0.0076)。
Table 5.
Logistic Univariate and Multivariate Analysis of Predictors for pCR
pCR 预测因素的 Logistic 单变量及多变量分析
| Univariate OR (97.5% CI) 单变量 OR(97.5% CI) |
p value p 值 | Multivariate OR (97.5% CI) 多变量 OR(97.5% CI) |
p value p 值 | |
|---|---|---|---|---|
| Age (>64.5 vs ≤64.5) 年龄(>64.5 vs ≤64.5) | 0.771 (0.372, 1.587) | 0.4808 | ||
| Sex (Male vs Female) 性别(Male vs Female) | 1.127 (0.512, 2.606) | 0.7713 | ||
| Smoking history (Yes/No) 吸烟史(Yes/No) | 2.012 (0.765, 5.121) | 0.1149 | ||
|
Drinking history (Yes/No) 饮酒史(Yes/No) |
1.387 (0.568, 3.239) | 0.4574 | ||
|
Hypertension history (Yes/No) 高血压病史(Yes/No) |
1.048 (0.462, 2.288) | 0.9074 | ||
|
Diabetes history (Yes/No) 糖尿病病史(Yes/No) |
2.184 (0.517, 8.686) | 0.2630 | ||
| CHD history (Yes/No) CHD 病史(Yes/No) | 2.757 (0.624, 12.204) | 0.1664 | ||
| Location 位置 | ||||
| Middle vs Upper 中部 vs 上部 | 1.164 (0.396, 3.925) | 0.7921 | ||
| Lower vs Upper 下部 vs 上部 | 1.463 (0.476, 5.094) | 0.5224 | ||
| cT Stage cT 分期 | ||||
| T3 vs T2 T3 对比 T2 | 0.623 (0.288, 1.339) | 0.2258 | ||
| T4 vs T2 T4 与 T2 | 0.300 (0.065, 1.024) | 0.0780 | ||
|
cN Stage (N+ vs N0) cN 分期(N+ vs N0) |
0.361 (0.155, 0.789) | 0.0136 | ||
| cTNM Stage cTNM 分期 | ||||
| III vs II III 对比 II | 0.287 (0.099, 0.724) | 0.0125 | 0.330 (0.115, 0.942) | 0.0388 |
| IVA vs II | 0.184 (0.041, 0.580) | 0.0094 | 0.158 (0.041, 0.614) | 0.0076 |
| Differentiation 分化 | ||||
| Low vs High 低 vs 高 | 0.290 (0.066, 1.206) | 0.0905 | ||
| Medium vs High 中 vs 高 | 0.533 (0.171, 1.741) | 0.2798 | ||
| SITI | ||||
| 2 vs 1 2 对 1 | 0.347 (0.133, 0.867) | 0.0258 | 0.361 (0.134, 0.968) | 0.0437 |
| 3 vs 1 | 0.106 (0.038, 0.272) | <0.0001 | 0.104 (0.038, 0.290) | <0.0001 |
Abbreviations: pCR, pathological complete response; CHD, coronary heart disease; SITI, systemic inflammation-tumor markers index; OR, odds ratio; CI, confidence interval.
缩写:pCR,病理完全缓解;CHD,冠心病;SITI,全身炎症-肿瘤标志物指数;OR,比值比;CI,置信区间。
Nomogram Constructed to Predict pCR and Validated
用于预测 pCR 的列线图构建及验证
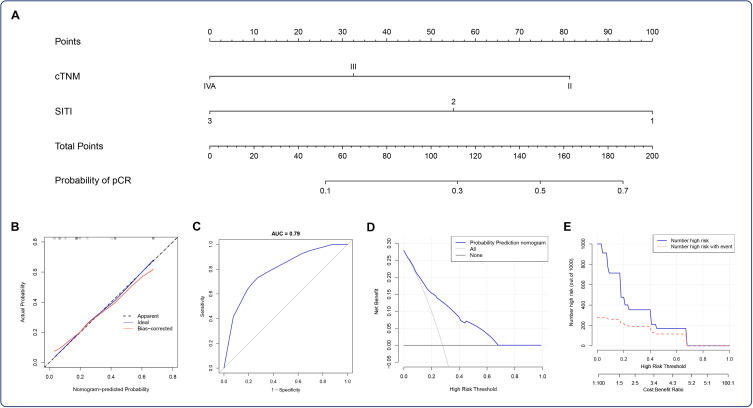
Finally, we established a nomogram to predict pCR according to the independent predictors (SITI and cTNM) identified in the multivariate stepwise forward logistic regression analyses (Figure 4A). To better understand the predictive value of the nomogram, the calibration slope and the ROC were also plotted to graphically assess calibration and discrimination, respectively (Figure 4B and C). The decision curve (Figure 4D) and the clinical impact curve (Figure 4E) for this model was performed and indicated a good clinical applicability in predicting the probability of pCR. These results confirmed that the SITI-based nomogram may serve as a simple and potential model for predicting pCR in resectable LA-ESCC treated with nICT.
最终,我们根据多变量逐步前向 Logistic 回归分析中确定的独立预测因子(SITI 和 cTNM)建立了预测 pCR 的列线图( Figure 4A )。为更好理解该列线图的预测价值,通过绘制校准曲线( Figure 4B )和 ROC 曲线( C )分别评估校准度与区分度。该模型的决策曲线( Figure 4D )和临床影响曲线( Figure 4E )显示其具有较好的临床应用价值。这些结果证实基于 SITI 的列线图可作为预测接受新辅助免疫化疗的局部晚期可切除食管鳞癌患者 pCR 的潜在简易模型。
Figure 4. 图 4.
Nomogram for pCR prediction. (A) A nomogram based on SITI and cTNM was established to predict pCR after nICT. (B) Calibration of the nomogram used to predict pCR. (C) ROC indicated an acceptable agreement regarding pCR prediction. The DCA (D) and clinical impact curve (E) indicated a good clinical applicability of the model in predicting the probability of pCR.
pCR 预测列线图。(A)基于 SITI 和 cTNMT 构建列线图预测 nICT 后 pCR。(B)用于预测 pCR 的列线图校准曲线。(C)ROC 曲线显示 pCR 预测一致性良好。DCA(D)和临床影响曲线(E)表明该模型在预测 pCR 概率方面具有良好的临床适用性。
Discussion 讨论
nICT is currently recommended only for clinical studies of esophageal cancer.7,8,15–17 In clinical practice, nICT brings higher pCR rates, but lacks effective markers. Therefore, it is of great significance to find more reliable indicators and establish more practical predictive models to guide personalized therapy for LA-ESCC patients. Evidence have suggested that several inflammatory indexes at baseline, including LY, NLR, PLR, LMR, and SII, were associated with pCR and prognosis after neoadjuvant therapy for esophageal cancer.20–22,24 We are the first to explore the dynamic changes of inflammatory indexes in resectable LA-ESCC patients before treatment, after nICT, and after surgical treatment. We found that the six included indicators, NEUT, LY, MONO, NLR, AISI and SII, were significantly decreased after surgery compared with those before treatment. Then the same phenomena were also observed in patients who achieved pCR. Moreover, the results showed that LMR significantly decreased after nICT and increased after surgery in patients achieving pCR.
目前 nICT 仅推荐用于食管癌的临床研究。 7 8 15–17 临床实践中 nICT 虽能带来更高的 pCR 率,但缺乏有效标志物。因此寻找更可靠的指标并建立更具实用性的预测模型以指导 LA-ESCC 患者个体化治疗具有重要意义。证据表明基线期多项炎症指标(LY、NLR、PLR、LMR、SII)与食管癌新辅助治疗后 pCR 及预后相关。 20–22 24 我们首次探讨了可切除 LA-ESCC 患者治疗前、nICT 后及术后炎症指标的动态演变规律,发现 NEUT、LY、MONO、NLR、AISI 及 SII 六个指标术后较治疗前显著降低,且在达到 pCR 的患者中也观察到同样现象。此外研究显示 pCR 患者 LMR 在 nICT 后显著下降,术后又明显回升。
Considering pCR as an important therapeutic effect and prognostic indicators of neoadjuvant therapy, further research was conducted on the predictive value of inflammatory indicators for pCR. We observed no significant differences in inflammation and nutritional markers between the pCR and non-pCR groups at baseline and after surgery. An interesting result, however, was that the pCR group had lower LMR and higher MONO after nICT treatment. Pre-treatment monocytes have been reported to be associated with immunotherapy.29 At present, we have no previous literature reports to support this result in our study. MONO is known to participate in phagocytosis, the removal of injured and senescent cells, as well as immune response and antigen presentation, which may explain this phenomenon to some extent.30,31 Tumor markers, including CA125,32 CEA,33,34 and CA155,34 have been reported to be associated with poor prognosis in esophageal carcinoma. Further, we attempted to use hematological indicators before treatment and after nICT to developed a novel scoring system based on inflammatory and tumor markers. Our results indicated that both SITI and cTNM were independent predictors of pCR in resectable LA-ESCC patients treated with nICT. Finally, we constructed a new nomogram based on SITI and cTNM that had good predictive ability for pCR.
将 pCR 作为新辅助治疗的重要疗效及预后指标,进一步研究了炎症指标对 pCR 的预测价值。我们观察到 pCR 组与非 pCR 组在基线及术后各炎症与营养指标均无显著差异。但有趣的是,pCR 组在 nICT 治疗后具有更低的 LMR 与更高的 MONO。已有研究报道治疗前单核细胞与免疫治疗相关 29 。但目前我们尚未检索到既往文献报道支持本研究该结果。已知 MONO 参与吞噬作用、清除损伤衰老细胞及免疫应答和抗原提呈,这可能在一定程度上解释该现象 30 31 。肿瘤标志物包括 CA125 32 、CEA 33 34 及 CA155 34 已被报道与食管癌预后不良相关。进一步地,我们尝试利用治疗前及 nICT 后的血液学指标构建基于炎症与肿瘤标志物的新型评分系统。 我们的结果表明,在接受新辅助化疗(nICT)治疗的可切除 LA-ESCC 患者中,SITI 和 cTNM 均是 pCR 的独立预测因素。最终我们基于 SITI 和 cTNM 构建了一种新的列线图,该模型对 pCR 具有良好的预测能力。
With the advent of a new era of precision immunotherapy, immunocheckpoint inhibitor therapy targeting the PD-1/PD-L1 pathway has revolutionized the treatment of esophageal cancer. Multiple Phase III clinical studies have established the role of immunotherapy in the first-line or second-line treatment of advanced esophageal squamous cell carcinoma.35,36 Immunotherapy combined with chemotherapy as neoadjuvant therapy has also been tried to be applied to locally advanced esophageal squamous cell carcinoma, in which efficacy and safety have also been observed.16,37–39 PDL1 expression, tumor mutation load, microsatellite stability, and T cell function were reported to be correlated with the efficacy of immunotherapy.18,19 However, due to medical conditions and economic factors, these tests are still difficult for some patients. Currently, finding the effective markers to predict treatment response is critical to precision therapy. Reports has aroused our concern that inflammatory markers, which are economical and convenient, are related to pCR and prognosis after neoadjuvant therapy in malignant tumors.20–23 Currently, there are few studies using inflammatory indicators to predict the pCR for nICT in LA-ESCC. We compared the predictive ability of our model to Feng Jifeng’s model.40 They constructed an IINS with eight indicators at baseline that the AUC for pCR was 0.7. SITI, which we constructed based on five indicators before and after nICT, seemed to have a higher predictive power for pCR (AUC=0.734). And our nomogram can predict pCR for nICT in resectable LA-ESCC (C-index=0.79), excellently. Another study, involving 64 patients, focused only on the predictive power of inflammation and nutritional indexes for pCR at baseline and after different treatment cycles.41 Compared to the other study,24 our study considered changes in hematological indicators before and after nICT treatment and constructed an entirely new model.
随着精准免疫治疗新时代的到来,以 PD-1/PD-L1 通路为靶点的免疫检查点抑制剂治疗为食管癌治疗带来了革命性改变。多项 III 期临床研究确立了免疫治疗在晚期食管鳞癌一线或二线治疗中的作用。 35 36 免疫治疗联合化疗作为新辅助治疗也尝试应用于局部晚期食管鳞癌,其中疗效及安全性也得到观察。 16 37–39 研究报道 PDL1 表达、肿瘤突变负荷、微卫星稳定性及 T 细胞功能与免疫治疗的疗效相关。 18 19 但由于医疗条件及经济因素,这些检测对于部分患者仍存在困难。目前寻找有效的标记物预测治疗反应对精准治疗至关重要。有报道引起了我们的关注,经济便捷的炎症标志物与恶性肿瘤新辅助治疗后 pCR 及预后相关。 20–23 目前,利用炎症指标预测 nICT 治疗 LA-ESCC 患者 pCR 的研究较少。我们将本模型的预测能力与冯继锋教授团队模型进行对比。 40 他们基于基线期八项指标构建的 IINS 评分系统预测 pCR 的 AUC 为 0.7。本研究基于 nICT 治疗前后五指标构建的 SITI 评分系统对 pCR 的预测效能更高(AUC=0.734),且列线图模型对可切除 LA-ESCC 患者 nICT 治疗后的 pCR 具有良好预测价值(C-index=0.79)。另一项纳入 64 例患者的研究仅关注基线期及不同治疗周期后炎症营养指标对 pCR 的预测效能。 41 与其他研究相比, 24 本研究通过观察 nICT 治疗前后血液学指标变化构建了全新预测模型。
Furthermore, our study still has some limitations. As a single-center retrospective study, there is a potential for bias in data collection. In this study, we mainly included 147 patients with resectable LA-ESCC who received 2 cycles of neoadjuvant therapy. As currently neoadjuvant immunochemotherapy is only recommended in clinical studies, the number of patients applying this regimen is limited, which also leads to the lack of external validation in this study. Although two studies found that prolonged nICT may lead to better pathological responses.42,43 However, Hongsheng Deng et al also found in the study that for the patients with stable disease/progressive disease (SD/PD) after neoadjuvant therapy, the benefit of pathological remission from additional cycles was relatively insignificant compared with the patients with significant therapeutic effect and partial response.42 In current clinical practice and research, the number of treatment cycles of nICT for patients with resectable LA-ESCC is still controversial, and it is unclear whether giving more treatment cycles is associated with better prognosis. Too few treatment cycles may lead to poor curative effect. Longer treatment cycles not only lead to higher treatment costs, but also may increase surgical risks. We ultimately decided to include the population who received 2 cycles of nICT, but this may have resulted in a certain selection bias. In the future we look forward to gaining more evidence to explore the best neoadjuvant therapy cycle. Additionally, due to the limited or absence of hematological markers in our cohort, we were unsuccessful in replicating other models. And the mechanisms affecting inflammation and nutritional indicators need further investigation. Despite the above limitations, the SITI-based nomogram may serve as a promising predictor to accurately and effectively differentiate pCR for nICT in resectable LA-ESCC patients.
此外,本研究仍存在一定局限性。作为一项单中心回顾性研究,可能存在数据收集偏倚。本研究主要纳入了 147 例接受 2 周期新辅助治疗的可切除 LA-ESCC 患者。由于目前新辅助免疫化疗仅在临床研究中推荐应用,采用该方案的患者数量有限,这也导致本研究缺乏外部验证。尽管两项研究发现延长 nICT 周期可能会带来更好的病理反应 42 43 。但 Hongsheng Deng 等在研究中也发现,对于新辅助治疗后疾病稳定/进展(SD/PD)患者,相较于疗效显著的部分缓解患者,追加周期带来的病理缓解获益相对有限 42 。在当前临床实践与研究中,可切除 LA-ESCC 患者接受 nICT 的治疗周期数仍存在争议,且尚不清楚给予更多治疗周期是否与更好预后相关。治疗周期过少可能导致疗效欠佳。 较长的治疗周期不仅导致更高的治疗成本,还可能增加手术风险。我们最终决定纳入接受 2 周期 nICT 的人群,但这可能导致一定的选择偏倚。未来我们期待获得更多证据以探索最佳新辅助治疗周期。此外,由于队列中血液学标志物数据有限或缺失,我们未能成功复现其他模型。影响炎症和营养指标的机制仍需进一步研究。尽管存在上述局限性,基于 SITI 的列线图仍可能作为一种有前景的预测工具,可精准有效地区分可切除 LA-ESCC 患者接受 nICT 后的 pCR。
Conclusion 结论
In summary, we are the first to explore the dynamic changes of inflammatory indexes in resectable LA-ESCC patients before treatment, after nICT, and after surgical treatment. We identified key indexes before and after nICT and constructed a predictive index named SITI. The SITI is an independent predictor for pCR in resectable LA-ESCC patients received nICT. The SITI-based nomogram may be a promising predictor to effectively differentiate pCR for nICT in resectable LA-ESCC patients, which has important implications for individualized treatment strategies.
总之,我们首次探讨了可切除 LA-ESCC 患者治疗前、nICT 后及术后炎症指标的动态演变规律,筛选出 nICT 前后关键指标并构建了 SITI 预测指标。SITI 是接受 nICT 治疗的可切除 LA-ESCC 患者获得 pCR 的独立预测因子,基于 SITI 的列线图模型能有效区分 nICT 后 pCR 状态,对制定个体化治疗策略具有重要参考价值。
Acknowledgments 致谢
The authors thank the participating patients for all their help in enabling completion of this study.
作者感谢所有参与患者对完成本研究提供的帮助。
Funding Statement 资助声明
This work was supported by the General program of National Natural Science Foundation of China (81672442), Natural Science Foundation of Henan Province (222300420557), Beijing Xisike Clinical Oncology Research Foundation (Y-HR2018-219).
本工作由国家自然科学基金面上项目(81672442)、河南省自然科学基金(222300420557)、北京希思科临床肿瘤学研究基金会(Y-HR2018-219)资助。
Ethics Approval and Consent to Participate
伦理批准与参与同意
This study was approved by the Ethics Committee of scientific research and clinical trial of the First Affiliated Hospital of Zhengzhou University (KY-2022-0362). All patients provided written-informed consent for the collection and publication of their medical information at the first visit to our center, which was filed in their medical records, and the ethics committees approved this consent procedure. The study complied with the Declaration of Helsinki.
本研究经郑州大学第一附属医院科研和临床试验伦理委员会(KY-2022-0362)批准。所有患者在首次就诊时均签署了关于收集和发布其医疗信息的书面知情同意书,该文件已存入其病历档案,且该知情同意程序获得伦理委员会批准。本研究遵循《赫尔辛基宣言》要求。
Disclosure 披露
The authors declare that they have no competing interests in this work.
作者声明,他们在本研究中无任何竞争性利益。
References 参考文献
-
1.Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390(10110):2383–2396. doi: 10.1016/s0140-6736(17)31462-9 [DOI] [PubMed] [Google Scholar]
1.Lagergren J、Smyth E、Cunningham D、Lagergren P. 食管癌。《柳叶刀》。2017;390(10110):2383–2396. doi: 10.1016/s0140-6736(17)31462-9 [ DOI ] [ PubMed ] [ Google Scholar ] -
2.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
2.Sung H、Ferlay J、Siegel RL 等。2020 年全球癌症统计:GLOBOCAN 对 185 个国家 36 种癌症全球发病率和死亡率的估算。CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660 [ DOI ] [ PubMed ] [ Google Scholar ] -
3.Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–1021. doi: 10.1007/s12328-020-01237-x [DOI] [PubMed] [Google Scholar]
3.Uhlenhopp DJ、Then EO、Sunkara T、Gaduputi V. 食管癌流行病学:全球趋势、病因及危险因素的最新进展. Clin J Gastroenterol. 2020;13(6):1010–1021. doi: 10.1007/s12328-020-01237-x [ DOI ] [ PubMed ] [ Google Scholar ] -
4.Ajani JA, D’Amico TA, Bentrem DJ, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(7):855–883. doi: 10.6004/jnccn.2019.0033 [DOI] [PubMed] [Google Scholar]
4.Ajani JA, D’Amico TA, Bentrem DJ, 等. 食管及食管胃结合部癌临床实践指南(2019.V2 版)[J]. 美国国立综合癌症网络杂志. 2019;17(7):855–883. doi: 10.6004/jnccn.2019.0033 [ DOI ] [ PubMed ] [ Google Scholar ] -
5.Hou S, Pan Z, Hao X, Hang Q, Ding Y. Recent progress in the neoadjuvant treatment strategy for locally advanced esophageal cancer. Cancers. 2021;13(20):5162. doi: 10.3390/cancers13205162 [DOI] [PMC free article] [PubMed] [Google Scholar]
5.Hou S, Pan Z, Hao X, Hang Q, Ding Y. 局部晚期食管癌新辅助治疗策略的最新进展. Cancers. 2021;13(20):5162. doi: 10.3390/cancers13205162 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
6.Yang H, Liu H, Chen Y, et al. Long-term efficacy of neoadjuvant chemoradiotherapy plus surgery for the treatment of locally advanced esophageal squamous cell carcinoma: the NEOCRTEC5010 randomized clinical trial. JAMA Surg. 2021;156(8):721–729. doi: 10.1001/jamasurg.2021.2373 [DOI] [PMC free article] [PubMed] [Google Scholar]
6.Yang H、Liu H、Chen Y 等. 新辅助放化疗联合手术治疗局部晚期食管鳞状细胞癌的长期疗效:NEOCRTEC5010 随机临床试验. JAMA Surg. 2021;156(8):721–729. doi: 10.1001/jamasurg.2021.2373 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
7.Yang H, Liu H, Chen Y, et al. Neoadjuvant chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the esophagus (NEOCRTEC5010): a phase III multicenter, randomized, open-label clinical trial. J Clin Oncol. 2018;36(27):2796–2803. doi: 10.1200/jco.2018.79.1483 [DOI] [PMC free article] [PubMed] [Google Scholar]
7.Yang H、刘 H、陈 Y 等。局部晚期食管鳞状细胞癌新辅助放化疗后手术与单纯手术的对比研究(NEOCRTEC5010):一项 III 期多中心、随机、开放标签临床试验。《临床肿瘤学杂志》。2018;36(27):2796–2803. doi: 10.1200/jco.2018.79.1483 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
8.Wang H, Tang H, Fang Y, et al. Morbidity and mortality of patients who underwent minimally invasive esophagectomy after neoadjuvant chemoradiotherapy vs neoadjuvant chemotherapy for locally advanced esophageal squamous cell carcinoma: a randomized clinical trial. JAMA Surg. 2021;156(5):444–451. doi: 10.1001/jamasurg.2021.0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
8.Wang H、Tang H、Fang Y 等. 新辅助放化疗与新辅助化疗后行微创食管切除术治疗局部晚期食管鳞状细胞癌患者的发病率和死亡率:一项随机临床试验. JAMA Surg. 2021;156(5):444–451. doi: 10.1001/jamasurg.2021.0133 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
9.Doki Y, Ajani JA, Kato K, et al. Nivolumab combination therapy in advanced esophageal squamous-cell carcinoma. N Engl J Med. 2022;386(5):449–462. doi: 10.1056/NEJMoa2111380 [DOI] [PubMed] [Google Scholar]
9.Doki Y、Ajani JA、Kato K 等。纳武利尤单抗联合疗法治疗晚期食管鳞状细胞癌。N Engl J Med. 2022;386(5):449–462. doi: 10.1056/NEJMoa2111380 [ DOI ] [ PubMed ] [ Google Scholar ] -
10.Luo H, Lu J, Bai Y, et al. Effect of camrelizumab vs placebo added to chemotherapy on survival and progression-free survival in patients with advanced or metastatic esophageal squamous cell carcinoma: the ESCORT-1st randomized clinical trial. JAMA. 2021;326(10):916–925. doi: 10.1001/jama.2021.12836 [DOI] [PMC free article] [PubMed] [Google Scholar]
10.Luo H、Lu J、Bai Y 等. 卡瑞利珠单抗对比安慰剂联合化疗治疗晚期或转移性食管鳞状细胞癌患者的总生存期和无进展生存期:ESCORT-1st 随机临床研究. JAMA. 2021;326(10):916–925. doi: 10.1001/jama.2021.12836 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
11.Wang ZX, Cui C, Yao J, et al. Toripalimab plus chemotherapy in treatment-naïve, advanced esophageal squamous cell carcinoma (Jupiter-06): a multi-center Phase 3 trial. Cancer Cell. 2022;40(3):277–288.e3. doi: 10.1016/j.ccell.2022.02.007 [DOI] [PubMed] [Google Scholar]
11.王泽旭、崔璨、姚俊等。特瑞普利单抗联合化疗治疗初治晚期食管鳞状细胞癌(JUPITER-06):一项多中心 III 期临床试验。癌细胞。2022;40(3):277–288.e3. doi: 10.1016/j.ccell.2022.02.007 [ DOI ] [ PubMed ] [ Google Scholar ] -
12.Lu Z, Wang J, Shu Y, et al. Sintilimab versus placebo in combination with chemotherapy as first line treatment for locally advanced or metastatic oesophageal squamous cell carcinoma (ORIENT-15): multicentre, randomised, double blind, phase 3 trial. BMJ. 2022;377:e068714. doi: 10.1136/bmj-2021-068714 [DOI] [PMC free article] [PubMed] [Google Scholar]
12.Lu Z, Wang J, Shu Y 等. 信迪利单抗对比安慰剂联合化疗一线治疗局部晚期或转移性食管鳞状细胞癌(ORIENT-15):多中心、随机、双盲、3 期临床试验. 英国医学杂志. 2022;377:e068714. doi: 10.1136/bmj-2021-068714 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
13.Sun JM, Shen L, Shah MA, et al. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–771. doi: 10.1016/s0140-6736(21)01234-4 [DOI] [PubMed] [Google Scholar]
13.孙 JM、沈 L、沙 MA 等. Pembrolizumab 联合化疗对比单纯化疗一线治疗晚期食管癌(KEYNOTE-590):一项随机、安慰剂对照的 3 期研究. 柳叶刀. 2021;398(10302):759–771. doi: 10.1016/s0140-6736(21)01234-4 [ DOI ] [ PubMed ] [ Google Scholar ] -
14.Wu Z, Zheng Q, Chen H, et al. Efficacy and safety of neoadjuvant chemotherapy and immunotherapy in locally resectable advanced esophageal squamous cell carcinoma. J Thorac Dis. 2021;13(6):3518–3528. doi: 10.21037/jtd-21-340 [DOI] [PMC free article] [PubMed] [Google Scholar]
14.Wu Z, Zheng Q, Chen H, et al. 新辅助化疗联合免疫治疗在局部可切除晚期食管鳞状细胞癌中的疗效与安全性. J Thorac Dis. 2021;13(6):3518–3528. doi: 10.21037/jtd-21-340 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
15.Liu J, Yang Y, Liu Z, et al. Multicenter, single-arm, Phase II trial of camrelizumab and chemotherapy as neoadjuvant treatment for locally advanced esophageal squamous cell carcinoma. J Immunother Cancer. 2022;10(3). doi: 10.1136/jitc-2021-004291 [DOI] [PMC free article] [PubMed] [Google Scholar]
15.Liu J、Yang Y、Liu Z 等. 卡瑞利珠单抗联合化疗作为局部晚期食管鳞状细胞癌新辅助治疗的多中心单臂 II 期试验. J Immunother Cancer. 2022;10(3). doi: 10.1136/jitc-2021-004291 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ] -
16.Liu J, Li J, Lin W, et al. Neoadjuvant camrelizumab plus chemotherapy for resectable, locally advanced esophageal squamous cell carcinoma (NIC-ESCC2019): a multicenter, Phase 2 study. Int J Cancer. 2022;151(1):128–137. doi: 10.1002/ijc.33976 [DOI] [PubMed] [Google Scholar]
16.Liu J、Li J、Lin W 等. 新辅助卡瑞利珠单抗联合化疗治疗可切除局部晚期食管鳞状细胞癌(NIC-ESCC2019):一项多中心 II 期研究. Int J Cancer. 2022;151(1):128–137. doi: 10.1002/ijc.33976 [ DOI ] [ PubMed ] [ Google Scholar ] - 17.Xing W, Zhao L, Zheng Y, et al. The sequence of chemotherapy and toripalimab might influence the efficacy of neoadjuvant chemoimmunotherapy in locally advanced esophageal squamous cell cancer-a phase II study. Front Immunol. 2021;12:772450. doi: 10.3389/fimmu.2021.772450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng H, Zhao Y, Cai X, et al. PD-L1 expression and tumor mutation burden as pathological response biomarkers of neoadjuvant immunotherapy for early-stage non-small cell lung cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2022;170:103582. doi: 10.1016/j.critrevonc.2022.103582 [DOI] [PubMed] [Google Scholar]
- 19.Lefler DS, Snook AE, Bashir B. Immune checkpoint inhibitors in luminal gastrointestinal malignancies: going beyond MSI-H/dMMR, TMB and PD-L1. Immunotherapy. 2022;14(11):885–902. doi: 10.2217/imt-2022-0012 [DOI] [PubMed] [Google Scholar]
- 20.Li Q, Zhou S, Liu S, et al. Treatment-related lymphopenia predicts pathologic complete response and recurrence in esophageal squamous cell carcinoma undergoing neoadjuvant chemoradiotherapy. Ann Surg Oncol. 2019;26(9):2882–2889. doi: 10.1245/s10434-019-07334-7 [DOI] [PubMed] [Google Scholar]
- 21.Wu Y, Chen J, Zhao L, et al. Prediction of pathologic response to neoadjuvant chemoradiotherapy in patients with esophageal squamous cell carcinoma incorporating hematological biomarkers. Cancer Res Treat. 2021;53(1):172–183. doi: 10.4143/crt.2020.594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li C, Lin JW, Yeh HL, Chuang CY, Chen CC. Good prediction of treatment responses to neoadjuvant chemoradiotherapy for esophageal cancer based on preoperative inflammatory status and tumor glucose metabolism. Sci Rep. 2021;11(1):11626. doi: 10.1038/s41598-021-90753-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai G, Yu J, Meng X. Predicting prognosis and adverse events by hematologic markers in patients with locally advanced esophageal squamous cell carcinoma treated with neoadjuvant chemoradiotherapy. Cancer Manag Res. 2020;12:8497–8507. doi: 10.2147/cmar.S257058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feng J, Wang L, Yang X, Chen Q, Cheng X. Prediction of pathologic complete response prediction in patients with locally advanced esophageal squamous cell carcinoma treated with neoadjuvant immunochemotherapy: a real-world study. Bosn J Basic Med Sci. 2022. doi: 10.17305/bjbms.2022.7696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rice TW, Patil DT, Blackstone EH. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: application to clinical practice. Ann Cardiothorac Surg. 2017;6(2):119–130. doi: 10.21037/acs.2017.03.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zinellu A, Collu C, Nasser M, et al. The Aggregate Index of Systemic Inflammation (AISI): a novel prognostic biomarker in idiopathic pulmonary fibrosis. J Clin Med. 2021;10(18):4134. doi: 10.3390/jcm10184134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li X, Zhang S, Lu J, Li C, Li N. The prognostic value of systemic immune-inflammation index in surgical esophageal cancer patients: an updated meta-analysis. Front Surg. 2022;9:922595. doi: 10.3389/fsurg.2022.922595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Budczies J, Klauschen F, Sinn BV, et al. Cutoff Finder: a comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS One. 2012;7(12):e51862. doi: 10.1371/journal.pone.0051862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shao Y, Lin S, Zhang P, et al. Baseline monocyte and its classical subtype may predict efficacy of PD-1/PD-L1 inhibitor in cancers. Biosci Rep. 2021;41(1). doi: 10.1042/bsr20202613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang L, Simons DL, Lu X, et al. Breast cancer induces systemic immune changes on cytokine signaling in peripheral blood monocytes and lymphocytes. EBioMedicine. 2020;52:102631. doi: 10.1016/j.ebiom.2020.102631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 2019;106(2):309–322. doi: 10.1002/jlb.4ri0818-311r [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao H, Chen W, Wu J, Wang L, Mao W. Clinical significance of preoperative serum tumor markers in esophageal squamous cell carcinoma. J Cancer Res Ther. 2014;10(Suppl):C179–85. doi: 10.4103/0973-1482.145863 [DOI] [PubMed] [Google Scholar]
- 33.Hong Z, Huang Z, Chen Z, Kang M. Prognostic value of carcinoembryonic antigen changes before and after operation for esophageal squamous cell carcinoma. World J Surg. 2022;46(11):2725–2732. doi: 10.1007/s00268-022-06672-0 [DOI] [PubMed] [Google Scholar]
- 34.Yang Y, Huang X, Zhou L, et al. Clinical use of tumor biomarkers in prediction for prognosis and chemotherapeutic effect in esophageal squamous cell carcinoma. BMC Cancer. 2019;19(1):526. doi: 10.1186/s12885-019-5755-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li ZC, Sun YT, Lai MY, Zhou YX, Qiu MZ. Efficacy and safety of PD-1 inhibitors combined with chemotherapy as first-line therapy for advanced esophageal cancer: a systematic review and network meta-analysis. Int Immunopharmacol. 2022;109:108790. doi: 10.1016/j.intimp.2022.108790 [DOI] [PubMed] [Google Scholar]
- 36.Zhu X, Shanzhou Q, Li D, Pang X, Ma D. PD-1 inhibitors versus chemotherapy as second-line treatment for advanced esophageal squamous cell carcinoma: a meta-analysis. BMC Cancer. 2021;21(1):1195. doi: 10.1186/s12885-021-08958-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shen D, Chen Q, Wu J, Li J, Tao K, Jiang Y. The safety and efficacy of neoadjuvant PD-1 inhibitor with chemotherapy for locally advanced esophageal squamous cell carcinoma. J Gastrointest Oncol. 2021;12(1):1–10. doi: 10.21037/jgo-20-599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang P, Zhou X, Yang X, et al. Neoadjuvant camrelizumab plus chemotherapy in treating locally advanced esophageal squamous cell carcinoma patients: a pilot study. World J Surg Oncol. 2021;19(1):333. doi: 10.1186/s12957-021-02446-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lv H, Tian Y, Li J, et al. Neoadjuvant sintilimab plus chemotherapy in resectable locally advanced esophageal squamous cell carcinoma. Front Oncol. 2022;12:864533. doi: 10.3389/fonc.2022.864533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feng J, Wang L, Yang X, Chen Q, Cheng X. Pathologic complete response prediction to neoadjuvant immunotherapy combined with chemotherapy in resectable locally advanced esophageal squamous cell carcinoma: real-world evidence from integrative inflammatory and nutritional scores. J Inflamm Res. 2022;15:3783–3796. doi: 10.2147/jir.S367964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang X, Gari A, Li M, et al. Combining serum inflammation indexes at baseline and post treatment could predict pathological efficacy to anti‑PD‑1 combined with neoadjuvant chemotherapy in esophageal squamous cell carcinoma. J Transl Med. 2022;20(1):61. doi: 10.1186/s12967-022-03252-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deng H, Liang H, Chen J, et al. Preoperative immunochemotherapy for locally advanced non-small cell lung cancer: an analysis of the clinical outcomes, optimal number of cycles, and peripheral immune markers. Transl Lung Cancer Res. 2022;11(12):2364–2381. doi: 10.21037/tlcr-22-439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Qiu F, Fan J, Shao M, et al.Two cycles versus three cycles of neoadjuvant sintilimab plus platinum-doublet chemotherapy in patients with resectable non-small-cell lung cancer (neoSCORE): a randomized, single center, two-arm phase II trial. ASCO Annual Meeting. 2022;2022. doi: 10.1200/JCO.2022.40.16_suppl.8500 [DOI] [Google Scholar]