Abstract 摘要
Background and Objectives: Odontogenic infections (OI) represent a frequent cause of dental and maxillo-facial interventions, mostly due to late presentations or misdiagnosed complications. It is believed that the intensity of the immunoinflammatory response in OI is the main prognostic factor. Therefore, in this research, it was pursued to determine if the combination of C-reactive protein (CRP) and Neutrophil to Lymphocyte Ratio (NLR) (CRP-NLR) may serve as potential severity predictors in patients with odontogenic infections. Materials and Methods: A retrospective analysis on 108 patients hospitalized for odontogenic infections was conducted at the Department of Maxillofacial Surgery. Depending on the symptom severity scale, patients hospitalized with OI were divided into two equal groups based on infection severity (SS). Results: Patients with severe OI from Group B were associated more frequently with diabetes mellitus and smoking more often than those with a lower severity from Group A. In Group A, abscesses of odontogenic origin accounted for 70.4% of hospitalizations, while in Group B, abscesses and cellulitis were associated in 55.6% of cases (p-value < 0.001). The disease outcomes were more severe in Group B patients, where 22.2% of them developed sepsis, compared to 7.4% of Group A patients (p-value = 0.030). However, there was no significant difference in mortality rates. The SS and systemic immune inflammation index (SII) scores of Group B patients were substantially higher than Group A patients (13.6 vs. 6.1 for the SS score, p-value < 0.001), respectively, 2312.4 vs. 696.3 for the SII score (p-value < 0.001). All biomarker scores, including the CRP-NLR relationship, were considerably higher in Group B patients, with a median score of 341.4 vs. 79.0 in Group B (p-value < 0.001). The CRP-NLR association determined a 7.28-fold increased risk of severe OI. The receiver operating curve (ROC) analysis of CRP-NLR yielded an area under curve (AUC) value of 0.889, with high sensitivity (79.6%) and high specificity (85.1%), for predicting a severe odontogenic infection using biomarkers measured at hospital admission (p-value < 0.001). Conclusions: Therefore, it can be concluded that CRP-NLR is a reliable and affordable biomarker for determining the severity of odontogenic infections that may be included in other prognostic models for dental infections.
背景與目標:齒源性感染 (OI) 是牙科和顎面手術的常見原因,主要由於延遲就診或誤診的併發症。一般認為,OI 中免疫炎症反應的強度是主要預後因素。因此,本研究旨在確定 C 反應蛋白 (CRP) 與嗜中性白血球與淋巴球比率 (NLR) (CRP-NLR) 的組合是否可作為齒源性感染患者潛在的嚴重程度預測因子。材料與方法:對顎面外科住院的 108 名齒源性感染患者進行回顧性分析。根據症狀嚴重程度量表,將因 OI 住院的患者根據感染嚴重程度 (SS) 分為兩個相等的組別。結果:B 組的嚴重 OI 患者比 A 組的較低嚴重程度患者更常伴有糖尿病和吸煙。在 A 組中,齒源性膿瘍佔住院的 70.4%,而在 B 組中,膿瘍和蜂窩組織炎在 55.6% 的病例中相關 (p 值 < 0.001)。B 組患者的疾病結果更嚴重,其中 22.2% 的患者發生敗血症,而 A 組患者為 7.4% (p 值 = 0.030)。然而,死亡率沒有顯著差異。B 組患者的 SS 和全身免疫炎症指數 (SII) 評分顯著高於 A 組患者(SS 評分分別為 13.6 對 6.1,p 值 < 0.001),SII 評分分別為 2312.4 對 696.3(p 值 < 0.001)。所有生物標記評分,包括 CRP-NLR 關係,在 B 組患者中顯著較高,B 組的中位數評分為 341.4 對 79.0 (p 值 < 0.001)。CRP-NLR 關聯性確定了嚴重 OI 的風險增加了 7.28 倍。CRP-NLR 的接受者操作特徵曲線 (ROC) 分析產生的曲線下面積 (AUC) 值為 0.889,具有高靈敏度 (79.6%) 和高特異性 (85.1%),可用於預測入院時測量的生物標記的嚴重齒源性感染 (p 值 < 0.001)。結論:因此,可以得出結論,CRP-NLR 是一種可靠且經濟實惠的生物標記,可用於確定齒源性感染的嚴重程度,並且可以包含在其他牙科感染的預後模型中。
Keywords: inflammatory markers, disease severity score, odontogenic infections
關鍵詞:炎症標記物、疾病嚴重程度評分、齒源性感染
1. Introduction 1. 緒論
Overall, the incidence of severe odontogenic infections is believed to be declining for a variety of reasons, including the availability of antimicrobials, innovations in healthcare delivery, and overall improvement in oral hygiene, leading to a decrease in mortality [1,2]. Infections of dental origin are rather prevalent, with some studies claiming they account for a significant percentage of antibiotic prescriptions. However, if left untreated, they might extend to the maxillofacial and cervical regions, hence posing a plethora of potential concerning issues [3,4].
總體而言,由於多種原因,包括抗菌藥物的可用性、醫療保健服務的創新以及口腔衛生的總體改善,嚴重齒源性感染的發生率被認為正在下降,從而導致死亡率的降低[1, 2]。牙源性感染相當普遍,一些研究聲稱它們佔抗生素處方的重要百分比。然而,如果不及時治療,它們可能會擴散到頜面部和頸部區域,因此會帶來許多潛在的令人擔憂的問題[3, 4]。
It is crucial while treating patients with odontogenic infections to identify those that pose a high likelihood of developing serious consequences. These results may influence judgments on the dosage and effectiveness of therapy for some complicated cases. The strength of the immunoinflammatory response is believed to be a main prognostic factor [5]. Using factors derived from basic blood tests, several scores have been developed to predict the duration and severity of infections [6]. Such characteristics would be especially beneficial due to their quick availability and inexpensive cost. White blood cell (WBC) count, Neutrophil to Lymphocyte Ratio (NLR), and C-reactive protein are a few examples of (CRP) that were examined as objective assessment factors, but the findings were inconsistent [7,8,9].
在治療齒源性感染患者時,識別出那些極有可能產生嚴重後果的患者至關重要。這些結果可能會影響對某些複雜病例的治療劑量和有效性的判斷。免疫炎症反應的強度被認為是一個主要的預後因素[5]。利用來自基本血液檢查的因素,已經開發出幾種評分方法來預測感染的持續時間和嚴重程度[6]。由於這些特徵的快速可用性和低廉的成本,它們將特別有益。白血球(WBC)計數、中性粒細胞與淋巴細胞比率(NLR)和 C 反應蛋白(CRP)是一些被檢查作為客觀評估因素的例子,但研究結果並不一致[7, 8, 9]。
Consequently, the white blood cell count (WBC) is a well-researched predictor of inflammation [10] with a half-life of 5–6 days. However, due to CRP’s fast peaks and falls, it is a more sensitive marker for the course of infection than WBC [11]. In addition, WBC count levels alone were inadequate to rule in or rule out the existence of infections [12]. However, increased levels are vague and have little diagnostic accuracy. For instance, WBCs have a minimal role in the diagnosis and severity assessment of head and neck infections [13]; their significance lies mainly in the evaluation of the patient’s response to therapy. In comparison to odontogenic infections, CRP is a better infection measure than WBC because its level rises more rapidly [14,15,16]. CRP is present in minute quantities in healthy persons, increases quickly with infection within a few hours [17], and then rapidly decreases when the inflammation subsides. Due to the tight relationship between the intensity and duration of acute infections, CRP is a sensitive indicator of inflammatory processes. Due to this, CRP is often utilized as a marker for odontogenic infection, which corresponds with hospital length of stay [18], while some authors believe it will never become a diagnostic tool on its own but can only be evaluated in conjunction with other clinical and pathological findings [19].
因此,白血球計數 (WBC) 是一個經過充分研究的炎症預測因子 [ 10],半衰期為 5–6 天。然而,由於 CRP 的快速峰值和下降,它比 WBC 更能靈敏地反映感染的過程 [ 11]。此外,單獨的 WBC 計數水平不足以排除或確定感染的存在 [ 12]。然而,增加的水平是模糊的,並且幾乎沒有診斷準確性。例如,WBC 在頭頸部感染的診斷和嚴重程度評估中作用不大 [ 13];它們的意義主要在於評估患者對治療的反應。與牙源性感染相比,CRP 是一種比 WBC 更好的感染指標,因為它的水平上升得更快 [ 14, 15, 16]。CRP 在健康人體內含量極少,在感染後數小時內迅速增加 [ 17],然後在炎症消退時迅速下降。由於急性感染的強度和持續時間之間存在密切關係,CRP 是炎症過程的敏感指標。因此,CRP 通常被用作牙源性感染的標記,這與住院時間長度有關 [ 18],而一些作者認為它永遠不會成為一種獨立的診斷工具,只能與其他臨床和病理學發現一起評估 [ 19]。
Instead, the NLR score, computed as the ratio between the neutrophil and lymphocyte counts detected in peripheral blood, is a valid indicator for detecting inflammatory status, bacteremia, and sepsis [20,21]. Because the early hyperdynamic phase of infection is characterized by a proinflammatory state mediated by neutrophils, an isolated increase in neutrophil count, and thus, an elevated NLR, can be observed in a variety of conditions, including bacterial or fungal infection, acute stroke, myocardial infarction, atherosclerosis, severe trauma, malignancies, post-surgical complications, or any condition that can activate systemic inflammatory response syndrome (SIRS) [22,23,24,25,26,27,28]. NLR is a simple, fast-reacting, and generally accessible indicator of stress and inflammation with high sensitivity but limited specificity [29]. It is frequently employed in practically all medical fields nowadays, including emergency care, surgical fields, and infections in the craniofacial area; however, it is the subject of relatively insufficient research [30].
相反,NLR 評分,計算方法為周圍血液中檢測到的中性粒細胞和淋巴細胞計數之比,是檢測炎症狀態、菌血症和敗血症的有效指標 [20, 21]。由於感染的早期高動力階段的特徵是由中性粒細胞介導的促炎狀態,因此在多種情況下可以觀察到中性粒細胞計數的孤立性增加,從而導致 NLR 升高,包括細菌或真菌感染、急性中風、心肌梗塞、動脈粥樣硬化、嚴重創傷、惡性腫瘤、術後併發症或任何可以激活全身炎症反應綜合徵 (SIRS) 的情況 [22, 23, 24, 25, 26, 27, 28]。NLR 是一種簡單、快速反應且通常易於獲得的壓力和炎症指標,具有高敏感性但特異性有限 [29]。如今,它幾乎被應用於所有醫療領域,包括急診護理、外科領域和顱面區域的感染;然而,對它的研究相對不足 [30]。
Neutrophil to lymphocyte ratio (NLR) and C-reactive protein (CRP) levels are typically elevated in patients that develop abnormal inflammatory responses. To our knowledge, no studies have investigated so far the relationship between NLR and CRP with the severity of odontogenic infections. Therefore, it is believed that combining these two inflammatory scores would result in a more accurate disease-severity score, while the null hypothesis states that NLR-CRP association is an insignificant predictor of OI severity. In our investigation, we predicted that by combining the fast-rising characteristics of CRP with the high sensitivity of NLR for inflammation, it would be possible to obtain a measure with the capacity to predict the severity of odontogenic infections with great accuracy.
中性粒細胞與淋巴細胞比率 (NLR) 和 C-反應蛋白 (CRP) 水平通常在發生異常炎症反應的患者中升高。據我們所知,目前還沒有研究調查 NLR 和 CRP 與牙源性感染嚴重程度之間的關係。因此,我們認為結合這兩個炎症評分可以產生更準確的疾病嚴重程度評分,而虛無假設表明 NLR-CRP 關聯性對於預測牙源性感染的嚴重程度並不重要。在我們的研究中,我們預測通過將 CRP 的快速上升特性與 NLR 對炎症的高敏感性相結合,可以獲得一種能夠非常準確地預測牙源性感染嚴重程度的指標。
2. Materials and Methods
2. 材料與方法
2.1. Study Design and Ethics
2.1. 研究設計與倫理
The study was designed as a retrospective cohort of patients admitted for odontogenic infections to the Maxillofacial Surgery Department of City Emergency Hospital Timisoara (SCMUT), affiliated with the Victor Babes University of Medicine and Pharmacy from Timisoara between January 2017 to April 2022. These data were collected from digital and paper records only with the patient’s agreement and the ethical approval obtained from the Ethics Committee of SCMUT with the approval number I-27098 from 14 October 2022.
本研究設計為一項回顧性队列研究,研究對象為 2017 年 1 月至 2022 年 4 月期間因牙源性感染入院至蒂米什瓦拉市急診醫院(SCMUT)口腔頜面外科,該醫院隸屬於蒂米什瓦拉 Victor Babes 醫學與藥學大學。這些數據僅在徵得患者同意並獲得 SCMUT 倫理委員會的倫理批准(批准號 I-27098,日期為 2022 年 10 月 14 日)後,才從數位和紙質記錄中收集。
2.2. Patient Selection Process
2.2. 病患選擇流程
Patients above the age of eighteen were enrolled in the research. Infections of odontogenic origin were examined for inclusion according to the international classification of diseases (ICD-10) disease classification [31]. Patients whose medical records were incomplete were excluded from the research. Patients under the age of 18, pregnant women, and those with malignancy, immunodeficiency, or infections of origin other than odontogenic were excluded from the research, to avoid potential outliers in the levels of serum inflammatory markers. According to the Symptom Severity score (SS) presented in Table 1, eligible cases were divided into two groups based on the severity of the infection. The low-severity infection group consisted of mild to moderate infections, whereas the high-severity infection group included moderate to severe infections. At admission, the SS score of odontogenic infection created by Sainuddin et al. [30] and used in this study was calculated. Sepsis was defined by the recent guidelines in accordance with the sequential sepsis-related organ failure assessment score (SOFA) [32].
參與研究的對象為年滿十八歲的患者。根據國際疾病分類(ICD-10)疾病分類 [31],檢查牙源性感染以納入研究。醫療記錄不完整的患者被排除在研究之外。為了避免血清發炎指標水平出現潛在的異常值,研究排除了 18 歲以下的患者、孕婦以及患有惡性腫瘤、免疫缺陷或非牙源性感染的患者。根據表 1 中呈現的症狀嚴重程度評分(SS),符合條件的病例根據感染的嚴重程度分為兩組。低嚴重程度感染組包括輕度至中度感染,而高嚴重程度感染組包括中度至重度感染。入院時,計算了 Sainuddin 等人 [30] 創建並在本研究中使用的牙源性感染 SS 評分。敗血症的定義符合近期指南,依據連續性敗血症相關器官衰竭評估評分(SOFA)[32]。
Table 1. 表 1。
The Symptom Severity score (SS) of odontogenic infections.
牙源性感染的症狀嚴重程度評分 (SS)。
| Criteria 標準 | Score 分數 | Max Score 最高分數 | |
|---|---|---|---|
| Systemic Inflammatory 全身性炎症 Response Syndrome (SIRS) 全身性發炎反應症候群 (SIRS) |
Temperature > 38.3 °C 體溫 > 38.3 °C |
1 | 4 |
| Heart rate > 90 bpm 心率 > 90 bpm |
1 | ||
| RR 20/min | 1 | ||
| WBC < 4 or >12 × 109 WBC < 4 或 >12 × 10 9 |
1 | ||
| Trismus 牙關緊閉 | Moderate < 2 cm 中度 < 2 厘米 |
3 | 4 |
| Severe < 1 cm 嚴重 < 1 厘米 |
4 | ||
| Dysphagia 吞嚥困難 | Mild—able to swallow most foods 輕度——能夠吞嚥大多數食物 |
2 | 5 |
| Moderate—unable to swallow fluids 中度——無法吞嚥液體 |
4 | ||
| Severe—drooling saliva 重度——流口水 | 5 | ||
| Collection in 1 fascial space 單一筋膜腔積液 |
Low severity (canine, vestibular) 低嚴重程度(犬齒窩、前庭) |
1 | 5 |
| Moderate severity (buccal) 中等嚴重程度(頰部) |
2 | ||
| High severity (all other spaces) 高嚴重程度(所有其他腔隙) |
4 | ||
| Collection in 2 or more fascial spaces 收集在 2 個或更多筋膜間隙中 |
5 | ||
| Sign of dehydration (↓BP/↑Urea/↓Skin turgor) 脫水跡象(↓BP/↑尿素/↓皮膚彈性) |
1 | 2 | |
| Comorbidities: diabetes mellitus, immunocompromised status, known or suspected chronic alcohol misuser 併發症:糖尿病、免疫功能低下、已知或疑似長期酗酒者 |
1 | ||
| Total Score 總分 | 20 | ||
SIRS—Systemic Inflammatory Response Syndrome; BP—Blood Pressure; RR—Respiratory Rate; WBC—White Blood Cells.
SIRS—全身性發炎反應症候群;BP—血壓;RR—呼吸頻率;WBC—白血球。
A convenience sampling method was employed to calculate the appropriate sample size. Considering the incidence of OI in the general population ranges between 0.05% and 0.1% [33,34], the computed ideal sample size was 34 patients, using a 99% confidence level and a 1 margin of error. Between January 2017 and April 2022, a total of 141 eligible patients identified with odontogenic infections were hospitalized at the Maxillofacial Surgery Department of the SCMUT. After deleting missing data and filtering by severity scores, 108 patients were eventually matched 1:1 by severity index and included in the study. The records were subsequently divided into two groups based on the primary anatomic space involved and the SS score: Group A consists of 54 individuals with a lower severity (SS score from 0 to 8 points); Group B consists of 54 patients with a greater severity (SS score from 9 to 16 points).
採用便利抽樣方法計算合適的樣本量。 考慮到一般人群中齒源性感染的發病率在 0.05% 到 0.1% 之間 [ 33, 34],計算出的理想樣本量為 34 名患者,使用 99% 的置信水平和 1 的誤差範圍。 2017 年 1 月至 2022 年 4 月期間,共有 141 名符合條件且被診斷患有齒源性感染的患者在 SCMUT 的頜面外科住院。 在刪除缺失數據並按嚴重程度評分進行篩選後,最終將 108 名患者按嚴重程度指數 1:1 進行匹配,並納入研究。 隨後,根據主要受累的解剖空間和 SS 評分將記錄分為兩組:A 組由 54 名嚴重程度較低的個體組成(SS 評分為 0 到 8 分); B 組由 54 名嚴重程度較高的患者組成(SS 評分為 9 到 16 分)。
2.3. Data Collection and Variables
2.3. 數據收集和變量
Demographic data and the patient’s medical history were collected. The hospital information system obtained the patients’ discharge reports, clinical evaluations, laboratory values, and imaging tests. Furthermore, routine blood samples, white blood cell count (WBC), hemogram indexes such as neutrophil and lymphocyte count, Neutrophil to Lymphocyte Ratio (NLR), and platelet count were evaluated. The variables considered for analysis comprised demographic data: age, gender, and place of origin, clinical presentation features (body temperature, trismus (mild, moderate, or severe), odontalgia (visual analog scale), mandibular pain (visual analog scale), dysfunctional disturbances of the masticatory system (mandibular dysfunction, headache, and unilateral chewing side)), edema, signs of obstruction (dyspnea, dysphagia), and signs of systemic infection (temperature >38.3 °C or <35.3 °C, heart rate > 90 bpm, respiratory rate > 20/min, blood pressure and WBC < 4 or >12 × 10³/μL) [35]. Routine blood sample on admission to the hospital: complete blood count, C-reactive protein, erythrocyte sedimentation rate (ESR), blood glucose levels, sodium and potassium, creatinine, and the glomerular filtration rate, blood urea nitrogen (BUN), aspartate transaminase (AST), alanine transaminase (ALT), clotting time, and swab culture with antibiogram. Research variables for serum parameters included the Neutrophil to Lymphocytes Ratio (NLR) obtained by dividing absolute Neutrophil and Lymphocyte counts.
收集了人口統計數據和患者的病史。 醫院信息系統獲取了患者的出院報告、臨床評估、實驗室數值和影像學檢查。 此外,還評估了常規血樣、白細胞計數 (WBC)、血象指標(如嗜中性白血球和淋巴球計數)、嗜中性白血球與淋巴球比率 (NLR) 和血小板計數。 分析考慮的變量包括人口統計數據:年齡、性別和原籍地、臨床表現特徵(體溫、牙關緊閉(輕度、中度或重度)、牙痛(視覺模擬量表)、下頜疼痛(視覺模擬量表)、咀嚼系統功能障礙(下頜功能障礙、頭痛和單側咀嚼側))、水腫、阻塞徵象(呼吸困難、吞嚥困難)和全身感染徵象(體溫 >38.3 °C 或 <35.3 °C、心率 > 90 bpm、呼吸頻率 > 20 次/分鐘、血壓和 WBC < 4 或 >12 × 10³/μL)[ 35]。 入院時的常規血樣:全血細胞計數、C-反應蛋白、紅血球沉降率 (ESR)、血糖水平、鈉和鉀、肌酐和腎絲球過濾率、血尿素氮 (BUN)、天門冬胺酸轉胺酶 (AST)、丙胺酸轉胺酶 (ALT)、凝血時間和帶抗生素敏感試驗的拭子培養。 血清參數的研究變量包括通過將絕對嗜中性白血球和淋巴球計數相除獲得的嗜中性白血球與淋巴球比率 (NLR)。
2.4. Statistical Analysis
2.4. 統計分析
Data were obtained electronically and deidentified. Mean values and standard deviations (SD), p-values, and correlation coefficient “r” of the laboratory values were calculated using the statistical analysis software MedCalc (MedCalc Software bv, Ostend, Belgium). Variables were compared between group A and group B, including the laboratory tests mentioned above related to the Severity Score (SS) of odontogenic infections. The Mann−Whitney U test was applied to compare non-normally distributed means, while Student’s t-test was used to compare normally-distributed data. Chi-square and Fischer’s exact tests were applied to verify a possible difference between the two groups regarding variables described as proportionate values. Logistic regression analysis was applied to determine the association between CRP and NLR. The hazard ratio and adjusted odds ratios were determined for the assessment of CRP and NLR as predictors for infection severity (represented by SS score severity). The area under the curve (AUC) was plotted for CRP and NLR to determine their accuracy in predicting the severity of odontogenic infections. A p-value < 0.05 was considered statistically significant when comparing the study variables.
數據以電子方式獲取並去識別化。使用統計分析軟件 MedCalc(MedCalc Software bv,奧斯滕德,比利時)計算實驗室值的平均值和標準差 (SD)、p 值和相關係數“r”。比較 A 組和 B 組之間的變量,包括與牙源性感染嚴重程度評分 (SS) 相關的上述實驗室測試。 Mann−Whitney U 檢驗用於比較非正態分佈的均值,而 Student's t 檢驗用於比較正態分佈的數據。應用卡方檢驗和 Fischer 精確檢驗來驗證兩組之間在描述為比例值的變量方面是否存在可能的差異。應用邏輯回歸分析來確定 CRP 和 NLR 之間的關聯。確定風險比和調整後的勝算比,以評估 CRP 和 NLR 作為感染嚴重程度(以 SS 評分嚴重程度表示)的預測指標。繪製 CRP 和 NLR 的曲線下面積 (AUC),以確定它們在預測牙源性感染嚴重程度方面的準確性。當比較研究變量時,p 值 < 0.05 被認為具有統計學意義。
3. Results 3. 結果
3.1. Demographic Characteristics of the Study Population
3.1. 研究人群的人口統計學特徵
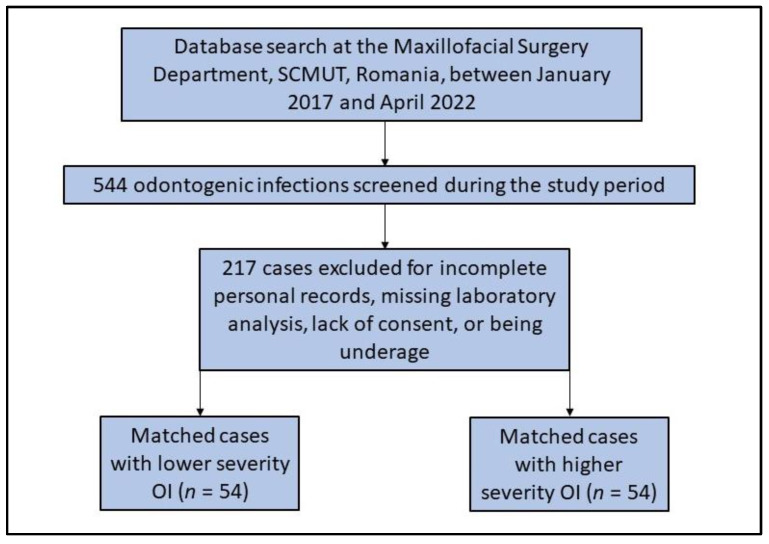
In total, 544 patients diagnosed clinically and radiologically with odontogenic infections were admitted and hospitalized at the Maxillofacial Surgery Department, SCMUT, Romania, between January 2017 and April 2022. Only 108 patients met the inclusion criteria and were enrolled in the study, as described in Figure 1. The patients were further subcategorized according to the SS score into two groups as follows: Group A—the low-severity infection group with 54 patients whose severity score ranges from 0 to 8 points on the SS scale; Group B—the high-severity infection group including 54 patients with a severity score between 9 and over 16 points. Table 2 describes the comparison of background characteristics among patients with odontogenic infections. It was observed that men were more frequently involved with OI (55.6% in Group A and 66.7% in Group B). The mean age was 46.7 years in Group A (age range 18–81), compared with 51.7 years in Group B (age range 20–85), without a statistically significant difference (p-value = 0.150). However, the place of origin was significantly different between the study groups, with patients with more severe infections coming more frequently from rural regions (68.5% vs. 46.3%, p-value = 0.019). Additionally, patients with severe OI were more often affected by diabetes mellitus (p-value < 0.001), and smoking was more common in Group B compared to the group with lower severity infections (35.2% vs. 16.7%, p-value = 0.028).
總共有 544 名經臨床和放射學診斷為牙源性感染的患者,於 2017 年 1 月至 2022 年 4 月期間在羅馬尼亞 SCMUT 的頜面外科部門入院和住院。只有 108 名患者符合納入標準並納入研究,如圖 1 所示。根據 SS 評分,患者進一步分為兩組,如下所示:A 組——低嚴重程度感染組,包含 54 名患者,其嚴重程度評分在 SS 量表上為 0 到 8 分;B 組——高嚴重程度感染組,包含 54 名患者,其嚴重程度評分為 9 分到超過 16 分。表 2 描述了牙源性感染患者背景特徵的比較。觀察到男性更常發生 OI(A 組為 55.6%,B 組為 66.7%)。A 組的平均年齡為 46.7 歲(年齡範圍 18-81 歲),而 B 組為 51.7 歲(年齡範圍 20-85 歲),無統計學顯著差異(p 值 = 0.150)。然而,研究組之間的原產地存在顯著差異,來自農村地區的患者更常患有更嚴重的感染(68.5% vs. 46.3%,p 值 = 0.019)。此外,患有嚴重 OI 的患者更常受到糖尿病的影響(p 值 < 0.001),並且與嚴重程度較低的感染組相比,B 組的吸煙更為常見(35.2% vs. 16.7%,p 值 = 0.028)。
Figure 1. 圖 1.
Patients’ inclusion flowchart.
病患納入流程圖。
Table 2. 表 2.
Comparison of background characteristics among patients with odontogenic infections.
比較牙源性感染患者的背景特徵。
| Variables 變數 | Group A (n = 54) A 組 (n = 54) |
Group B (n = 54) B 組 (n = 54) |
Significance 顯著性 |
|---|---|---|---|
| Gender 性別 | 0.236 | ||
| Men 男性 | 30 (55.6%) | 36 (66.7%) | |
| Women 女性 | 24 (44.4%) | 18 (33.3%) | |
| Age, mean (mean ± SD) 年齡,平均值(平均值 ± 標準差) |
46.7 ± 17.9 | 51.7 ± 18.1 | 0.150 |
| Age range 年齡範圍 | 18–81 | 20–85 | NA |
| Place of origin 產地 | 0.019 | ||
| Rural | 25 (46.3%) | 37 (68.5%) | |
| Urban 都市 | 29 (53.7%) | 17 (31.5%) | |
| Smoking 吸煙 | 0.028 | ||
| Yes 是 | 9 (16.7%) | 19 (35.2%) | |
| No 否 | 45 (83.3%) | 35 (64.8%) | |
| Comorbidities 合併症 | |||
| Diabetes mellitus 糖尿病 | 10 (18.5%) | 28 (51.9%) | <0.001 |
| Obesity 肥胖 | 31 (57.4%) | 37 (68.5%) | 0.231 |
| Chronic kidney disease 慢性腎臟病 | 14 (25.9%) | 17 (31.5%) | 0.523 |
| Malignancy 惡性腫瘤 | 5 (9.3%) | 7 (13.0%) | 0.540 |
| Others 其他 | 2 (3.7%) | 4 (7.4%) | 0.401 |
Data reported as n (%) and calculated using the Chi-square test and Fisher’s exact test unless specified differently; median and IQR values compared with Mann–Whitney u-test; IQR—Interquartile range.
除非另有说明,否则数据以 n (%) 形式报告,并使用卡方检验和 Fisher 精确检验计算;中位数和 IQR 值与 Mann-Whitney u 检验进行比较;IQR—四分位距。
3.2. Characteristics of Infection in the Study Population
3.2. 研究人群中感染的特征
Regarding the infection type in OI admitted to the hospital, 70.4% of them were abscesses in the lower infection cohort (Group A), while in Group B, 55.6% of infections were associations of abscesses and cellulitis (p-value < 0.001), as seen in Table 3. The most involved infection sites were the superficial lodges (40.7% vs. 48.1%), and peri-mandibular infections (25.9% vs. 33.3%), without statistically significant differences. Regarding disease outcomes, a total of 22.2% of patients in Group B developed sepsis, compared to 7.4% in Group A (p-value = 0.030), and four patients with severe OI were admitted to the ICU. However, mortality was not significantly different between the study groups (0.0% in Group A vs. 5.6% in Group B, p-value = 0.078). The median duration of hospitalization was significantly longer in patients from Group B, compared to Group A (12.0 days vs. 4.1 days, p-value < 0.001), in correlation with a higher frequency of severe complications in Group B (16.7% vs. 3.7%, p-value = 0.025).
至于因牙源性感染 (OI) 入院的感染类型,在较低感染队列(A 组)中,70.4% 为脓肿,而在 B 组中,55.6% 的感染是脓肿和蜂窝组织炎的结合(p 值 < 0.001),如表 3 所示。最常涉及的感染部位是浅表间隙(40.7% vs. 48.1%)和下颌周围感染(25.9% vs. 33.3%),没有统计学上的显着差异。关于疾病结果,B 组共有 22.2% 的患者发展为败血症,而 A 组为 7.4%(p 值 = 0.030),并且有 4 名患有严重 OI 的患者被送入 ICU。然而,研究组之间的死亡率没有显着差异(A 组为 0.0%,B 组为 5.6%,p 值 = 0.078)。与 A 组相比,B 组患者的平均住院时间明显更长(12.0 天 vs. 4.1 天,p 值 < 0.001),这与 B 组严重并发症发生率较高有关(16.7% vs. 3.7%,p 值 = 0.025)。
Table 3. 表 3.
Comparison of infection characteristics among patients with odontogenic infections.
比較牙源性感染患者的感染特性。
| Variables 變數 | Group A (n = 54) A 組 (n = 54) |
Group B (n = 54) B 組 (n = 54) |
Significance 重要性 |
|---|---|---|---|
| Reason for hospitalization 住院原因 |
<0.001 | ||
| Abscess 膿腫 | 38 (70.4%) | 17 (31.5%) | |
| Cellulitis 蜂窩組織炎 | 5 (9.3%) | 7 (13.0%) | |
| Association of abscess and cellulitis 膿腫與蜂窩組織炎的關聯 |
11 (20.4%) | 30 (55.6%) | |
| Infection site 感染部位 | |||
| Peri-maxillary 頜周圍 | 13 (24.1%) | 10 (18.5%) | 0.480 |
| Peri-mandibular 頜周圍 | 14 (25.9%) | 18 (33.3%) | 0.399 |
| Superficial lodges 表淺間隙 | 22 (40.7%) | 26 (48.1%) | 0.438 |
| Deep lodges 深層間隙 | 1 (1.9%) | 2 (3.7%) | 0.558 |
| Fascial 筋膜 | 5 (9.3%) | 3 (5.6%) | 0.462 |
| Outcomes 結果 | |||
| Sepsis 敗血症 | 4 (7.4%) | 12 (22.2%) | 0.030 |
| ICU admission 加護病房入住 | 0 (0.0%) | 4 (7.4%) | 0.041 |
| Duration of hospitalization, median (IQR) 住院時間,中位數(四分位距) |
4.1 (2.8) | 12.0 (5.7) | <0.001 |
| Severe complications 嚴重併發症 | 2 (3.7%) | 9 (16.7%) | 0.025 |
| Mortality 死亡率 | 0 (0.0%) | 3 (5.6%) | 0.078 |
Data reported as n (%) and calculated using the Chi-square test and Fisher’s exact test unless specified differently; median and IQR values compared with Mann-Whitney u-test; IQR—Interquartile range; ICU—Intensive care unit; SIRS—Systemic Inflammatory Response Syndrome.
除非另有說明,否則數據以 n (%) 形式報告,並使用卡方檢定和費雪精確檢定計算;中位數和 IQR 值使用 Mann-Whitney u 檢定進行比較;IQR—四分位距;ICU—加護病房;SIRS—全身性發炎反應症候群。
The symptom severity evaluation presented in Table 4 identified a total of 32 (59.2%) patients with a SIRS score ranging from 0 to 1 in Group A. On the other side, Group B patients were only 13 (24.0%) within the 0–1 score range (p-value < 0.001). A severe trismus score was observed in 27 (50.0%) of patients from Group B, compared to only 9.3% in Group A (p-value < 0.001). Similar observations were noticed in the dysphagia score and fascial space score, where a statistically significantly higher prevalence of high severity was found in Group B patients. The prevalence of patients with odontogenic infections who were admitted with dehydration and significant comorbidities was significantly higher in Group B (29.6% vs. 5.6% in Group A, p-value = 0.001).
表 4 中呈現的症狀嚴重程度評估顯示,A 組共有 32 名患者 (59.2%) 的 SIRS 評分範圍為 0 到 1。另一方面,B 組患者中只有 13 名 (24.0%) 的評分範圍在 0-1 之間(p 值 < 0.001)。 在 B 組患者中觀察到嚴重的牙關緊閉評分為 27 (50.0%),而 A 組僅為 9.3%(p 值 < 0.001)。 在吞嚥困難評分和筋膜間隙評分中也觀察到類似的現象,B 組患者中高嚴重程度的患病率在統計學上顯著較高。 B 組患者因牙源性感染入院時伴有脫水和顯著合併症的患者患病率顯著較高(B 組為 29.6%,A 組為 5.6%,p 值 = 0.001)。
Table 4. 表 4。
SS score differences among patients with odontogenic infections.
牙源性感染患者的 SS 評分差異。
| Variables 變量 | Group A (n = 54) A 組 (n = 54) |
Group B (n = 54) B 組 (n = 54) |
Significance 顯著性 |
|---|---|---|---|
| SIRS score 全身性炎症反應症候群評分 | <0.001 | ||
| 0 | 14 (25.9%) | 5 (9.2%) | |
| 1 | 18 (33.3%) | 8 (14.8%) | |
| 2 | 10 (18.5%) | 8 (14.8%) | |
| 3 | 6 (11.1%) | 19 (35.2%) | |
| 4 | 1 (1.8%) | 19 (35.2%) | |
| Trismus score 牙關緊閉評分 | <0.001 | ||
| Normal 正常 | 30 (55.6%) | 12 (22.2%) | |
| Moderate 中度 | 19 (35.2%) | 15 (27.8%) | |
| Severe 重度 | 5 (9.3%) | 27 (50.0%) | |
| Dysphagia score 吞嚥困難評分 | 0.028 | ||
| Normal 正常 | 5 (9.3%) | 18 (33.3%) | |
| Mild 輕微 | 21 (38.9%) | 16 (29.6%) | |
| Moderate 中等 | 17 (31.5%) | 29 (53.7%) | |
| Severe 嚴重 | 0 (0.0%) | 2 (3.7%) | |
| Fascial space score 筋膜腔間隙評分 | <0.001 | ||
| Low risk 低風險 | 39 (0.0%) | 10 (18.5%) | |
| Moderate risk 中等風險 | 23 (42.6%) | 27 (50.0%) | |
| Severe risk 嚴重風險 | 0 (0.0%) | 8 (14.8%) | |
| Dehydration/Comorbid 脫水/合併症 | 0.001 | ||
| No dehydration and comorbid 無脫水且無合併症 |
28 (51.9%) | 13 (24.1%) | |
| Dehydration or comorbid 脫水或合併症 | 26 (48.1%) | 22 (40.7%) | |
| Dehydration and comorbid 脫水且合併症 |
3 (5.6%) | 16 (29.6%) |
Data reported as n (%) and calculated using the Chi-square test and Fisher’s exact test unless specified differently; SS—Severity Score; SIRS—Systemic Inflammatory Response Syndrome.
數據以 n (%) 形式報告,並使用卡方檢驗和費舍爾精確檢驗計算,除非另有說明;SS—嚴重程度評分;SIRS—全身炎症反應綜合徵。
3.3. Risk Assessment in the Study Population
3.3. 研究人群的風險評估
Table 5 presents the comparison of severity scores and biomarker scores among patients with odontogenic infections admitted to the hospital. It was observed that SS and SII scores were statistically significantly higher among patients in Group B (13.6 vs. 6.1, p-value < 0.001), respectively, 2312.4 in Group B compared to 696.3 in Group A (p-value < 0.001). All tested biomarker scores were significantly higher in Group B patients, including the CRP-NLR association, with a median score of 341.4, compared with 79.0 in Group B (p-value < 0.001).
表 5 顯示了因牙源性感染入院的患者的嚴重程度評分和生物標誌物評分的比較。觀察到 B 組患者的 SS 和 SII 評分在統計學上顯著高於 A 組(分別為 13.6 vs. 6.1,p 值 < 0.001),B 組為 2312.4,而 A 組為 696.3(p 值 < 0.001)。所有測試的生物標誌物評分在 B 組患者中均顯著較高,包括 CRP-NLR 關聯,中位數評分為 341.4,而 B 組為 79.0(p 值 < 0.001)。
Table 5. 表 5.
Comparison of severity scores and biomarker scores among patients with odontogenic infections.
齒源性感染患者的嚴重程度評分與生物標記評分比較。
| Variables 變量 | Group A (n = 54) A 組(n = 54) |
Group B (n = 54) B 組(n = 54) |
Significance 顯著性 |
|---|---|---|---|
| Severity scores, (mean ± SD) 嚴重程度評分,(平均值 ± 標準差) |
|||
| SS | 6.1 ± 1.8 | 13.6 ± 3.9 | <0.001 * |
| SII | 696.3 ± 35.2 | 2312.4 ± 66.0 | <0.001 * |
| Biomarker scores (median, IQR) 生物標記分數(中位數,IQR) |
|||
| WBC, (median, IQR) 白血球 (中位數,四分位距) | 9.34 (7.92–11.50) | 12.02 (10.3–17) | <0.001 ** |
| WBC_Ne, (median, IQR) WBC_Ne,(中位數,四分位距) | 6.26 (4.68–10.23) | 8.05 (6.73–10.61) | 0.012 ** |
| WBC_Ly, (median, IQR) WBC_Ly,(中位數,四分位距) | 2.04 (1.41–2.7) | 2.56 (2.06–3) | 0.037 ** |
| NLR, (median, IQR) 中性粒細胞與淋巴細胞比率 (NLR),(中位數,四分位距) | 3.01 (2.10–4.83) | 3.31 (3–4.37) | 0.239 ** |
| CRP, (median, IQR) C 反應蛋白,(中位數,四分位距) | 22 (9–47) | 99 (86–118) | <0.001 ** |
| CRP-NLR, (median, IQR) CRP-NLR,(中位數,IQR) | 79.00 (22.14–191.4) | 341.47 (256.97–526.30) | <0.001 ** |
SD—standard deviation; SS—Severity Score; SII—Systemic Immune-Inflammation Index; WBC—White Blood Cells; WBC_Ne—White Blood Cells Neutrophils; WBC_Ly—White Blood Cells Lymphocytes; NLR—Neutrophil to Lymphocyte Ratio; CRP—C-Reactive Protein; * Student t-test; ** Kruskal–Wallis test; IQR—Interquartile Range.
SD—標準差;SS—嚴重程度評分;SII—全身免疫炎症指數;WBC—白血球;WBC_Ne—白血球嗜中性球;WBC_Ly—白血球淋巴球;NLR—嗜中性球與淋巴球比率;CRP—C 反應蛋白;* 學生 t 檢定;** Kruskal–Wallis 檢定;IQR—四分位距。
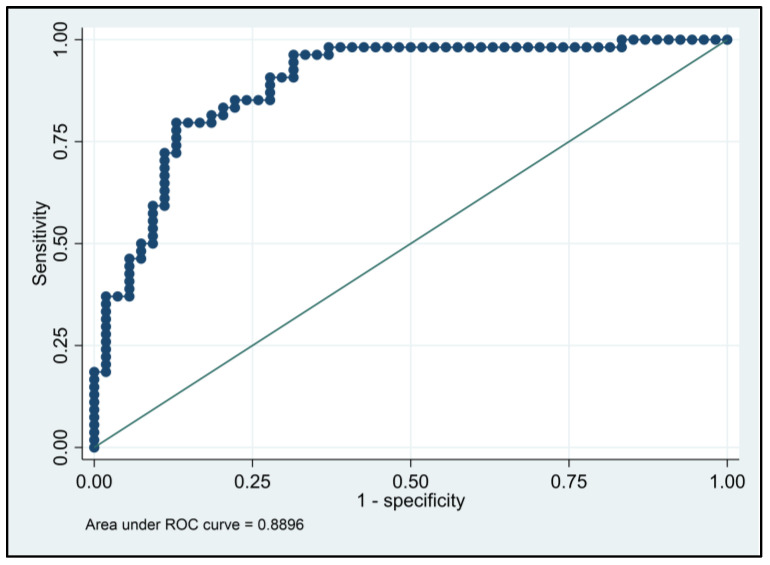
The logistic regression analysis presented in Table 6 describes the predictive of biological markers on the severity of odontogenic infections represented on the SS scale. It was observed that patients with an elevated WBC count had a 5.54 higher likelihood of severe OI, elevated neutrophils (OR = 7.10), elevated lymphocyte count (OR = 8.62), elevated NLR with an odds ratio of 4.46 (p-value < 0.001), high CRP levels with a 6.65 higher likelihood of severe OI, and lastly, the CRP-NLR association being responsible for a 7.28 higher risk (95% CI = 4.83–10.16). The ROC analysis of CRP-NLR resulted in a 0.889 AUC value (p-value < 0.001), with high sensitivity (79.6%) and high specificity (85.1%) for predicting a severe odontogenic infection using these biomarkers measured at hospital admission (Figure 2).
表 6 所示的邏輯回歸分析描述了生物標記物對 SS 量表上表示的齒源性感染嚴重程度的預測能力。觀察到白血球計數升高的患者患嚴重 OI 的可能性高 5.54 倍,嗜中性球升高(OR = 7.10),淋巴球計數升高(OR = 8.62),NLR 升高,優勢比為 4.46(p 值<0.001),高 CRP 水平患嚴重 OI 的可能性高 6.65 倍,最後,CRP-NLR 的關聯導致風險高 7.28 倍(95% CI = 4.83–10.16)。CRP-NLR 的 ROC 分析得出 0.889 的 AUC 值(p 值<0.001),具有高靈敏度(79.6%)和高特異性(85.1%),可用於預測入院時測量的這些生物標記物所導致的嚴重齒源性感染(圖 2)。
Table 6. 表 6。
Hazard ratios and adjusted odds ratio for SS score calculated at admission for predicting SIRS and sepsis after odontogenic infections.
用於預測牙源性感染後全身性炎症反應綜合徵和敗血症的入院時計算的 SS 評分的風險比和調整後勝算比。
| Variables 變量 | Risk (95% CI) 風險(95% CI) | Significance 顯著性 |
|---|---|---|
| SS (dependent variable) SS(因變量) | ||
| WBC | 5.54 (3.18–7.90) | <0.001 |
| WBC_Ne | 7.10 (5.19–9.01) | <0.001 |
| WBC_Ly | 8.62 (7.44–9.81) | <0.001 |
| NLR | 4.46 (3.53–5.40) | <0.001 |
| CRP | 6.65 (5.61–7.70) | <0.001 |
| CRP-NLR | 7.28 (4.83–10.16) | <0.001 |
Data were adjusted for age, comorbidities, and gender; WBC—White Blood Cells; WBC_Ne—White Blood Cells Neutrophils; WBC_Ly—White Blood Cells Lymphocytes; NLR—Neutrophil to Lymphocyte Ratio; CRP—C-Reactive Protein; CI—Confidence Interval.
數據已針對年齡、合併症和性別進行調整;WBC—白血球;WBC_Ne—白血球嗜中性球;WBC_Ly—白血球淋巴球;NLR—嗜中性球與淋巴球比率;CRP—C 反應蛋白;CI—信賴區間。
Figure 2. 圖 2。
ROC curve analysis of CRP-NLR.
CRP-NLR 的 ROC 曲線分析。
4. Discussion 4. 討論
4.1. Important Findings 4.1. 重要發現
The decision-making process in medicine incorporates clinical and laboratory considerations. Detecting an increase in acute phase reactants may assist the diagnostic interpretation of clinical symptoms in circumstances when an infection is suspected. In our investigation, CRP-NLR, which consists of CRP level at admission and NLR level at admission, was shown to have a more accurate ability to predict the severity of odontogenic infection. Initially, it was shown that a high CRP-NLR was substantially and strongly connected with high severity levels in odontogenic infection. Then, we examined the connection between CRP-NLR levels and WBC levels at admission in both severity groups and discovered that CRP-NLR had a greater predictive capability.
醫學上的決策過程包含臨床和實驗室的考量。當懷疑感染時,檢測急性期反應物的增加可能有助於臨床症狀的診斷解釋。在我們的研究中,CRP-NLR(包括入院時的 CRP 水平和入院時的 NLR 水平)顯示出更準確的預測牙源性感染嚴重程度的能力。最初,研究表明,高 CRP-NLR 與牙源性感染的高嚴重程度水平顯著且強烈相關。然後,我們檢查了 CRP-NLR 水平與兩個嚴重程度組的入院時的 WBC 水平之間的聯繫,並發現 CRP-NLR 具有更高的預測能力。
A better understanding of the inflammatory cascade has led to new discoveries and the identification of many mediators that, in combination with clinical symptoms, might serve as valuable infection indicators [36]. Bagul et al. [37] concluded in their study that CRP should be recommended as a monitoring marker for managing patients with fascial space infections of odontogenic origin, as it is a more sensitive indicator than WBC count and one of the best measuring tools for determining the infection control in these patients. In addition, John CR et al. [38] showed in their research analyzing indicators in patients with odontogenic fascial space infections that CRP should be suggested as a monitoring marker for the diagnosis of fascial space infection and for determining the response to treatment. In their research, Barreto et al. [39] found that the CRP test is a practical, easily accessible blood test that portrays the patient course and response to therapy more precisely than other commonly used indicators in oral and maxillofacial surgery.
對於炎症級聯反應的更深入理解,促成了新的發現,並確定了許多與臨床症狀相結合可能成為有價值的感染指標的介質[36]。Bagul 等人[37]在他們的研究中得出結論,建議將 CRP 作為監測標記,用於管理患有牙源性筋膜間隙感染的患者,因為它比 WBC 計數更敏感,並且是確定這些患者感染控制的最佳測量工具之一。此外,John CR 等人[38]在他們的研究中分析了牙源性筋膜間隙感染患者的指標,表明應將 CRP 作為監測標記,用於診斷筋膜間隙感染和確定對治療的反應。Barreto 等人[39]在他們的研究中發現,CRP 測試是一種實用且易於獲得的血液測試,與口腔頜面外科中其他常用的指標相比,它更準確地描述了患者的病程和對治療的反應。
Dynamic changes in NLR, on the other hand, predate the clinical condition by several hours and may alert doctors to an ongoing pathogenic process. Despite these benefits, NLR as a biomarker for assessing the progression of odontogenic infection has limited use. A recent meta-analysis [40] revealed that NLR was greater in non-survivors of sepsis than in survivors, and a larger NLR was linked with a worse prognosis in sepsis patients. Independent of the kind of operation (cardiac or abdominal), preoperative NLR levels are independent predictors of postoperative problems [41,42,43].
另一方面,NLR 的動態變化比臨床狀況早幾個小時出現,可能會提醒醫生注意正在進行的致病過程。儘管有這些好處,但 NLR 作為評估牙源性感染進展的生物標誌物的用途有限。最近的一項薈萃分析 [40] 顯示,非敗血症存活者的 NLR 高於敗血症存活者,而較高的 NLR 與敗血症患者的較差預後有關。與手術類型(心臟或腹部)無關,術前 NLR 水平是術後問題的獨立預測因子 [41, 42, 43]。
In addition, NLR may be used as a predictor for surgical treatment in submandibular abscesses [44] and as a recovery marker in odontogenic infection. Several investigations have demonstrated a correlation between NLR and the occurrence of pus, duration of hospital stay, and antibiotic dosage need [45]. In addition, the NLR value is constant and resistant to physiological and environmental factors, such as dehydration, physical exercise, and blood sample processing, that might influence test findings [46]. In their investigation, Dogruel et al. [47] determined that the NLR was related to hospitalization and antibiotic dosages in individuals with odontogenic infection. Incorporating the NLR into the CRP level has tremendous promise as a biomarker for odontogenic infection severity classification. Our objective was to determine whether CRP and NLR may serve as possible severity indicators in patients with odontogenic infections (OI).
此外,NLR 可用作頜下腺膿腫手術治療的預測因子 [ 44],以及牙源性感染的恢復指標。多項研究表明,NLR 與膿液的產生、住院時間和抗生素劑量需求之間存在相關性 [ 45]。此外,NLR 值穩定,且不受生理和環境因素的影響,如脫水、體力鍛鍊和血液樣本處理等,這些因素可能會影響測試結果 [ 46]。Dogruel 等人 [ 47] 在他們的研究中確定,NLR 與牙源性感染患者的住院治療和抗生素劑量有關。將 NLR 納入 CRP 水平中,作為牙源性感染嚴重程度分類的生物標誌物具有巨大的前景。我們的目標是確定 CRP 和 NLR 是否可以作為牙源性感染(OI)患者的潛在嚴重程度指標。
According to several research, despite the increase in frequency, the patient features have remained basically unchanged [48]. The majority of patients were in their mid-30s, which is much younger than the majority of patients in our research, who were in their mid-40s. Furthermore, the amount of time between the beginning of symptoms and hospital presentation stayed comparable in both groups, and the percentage of patients who sought dental treatment prior to hospitalization remained surprisingly high at more than 40%, despite the fact that our study lacks this type of information. In addition, almost two-thirds of patients reported in previous studies had been orally administered antibiotics by their dentist or primary care physician before presenting to the hospital, a number that increased from 57% to 63%. Instead of seeking to cure the underlying cause, it is considered that an over dependence on antibiotics results in suboptimal patient care. Therefore, the need for prediction scores and algorithms is essential to determine the patients at risk.
根據多項研究,儘管發生頻率有所增加,但患者的特徵基本上保持不變 [ 48]。大多數患者年齡在 30 多歲,遠低於我們研究中的大多數患者,他們的年齡在 40 多歲。此外,從症狀開始到入院的時間長度在兩組中保持相似,並且在入院前尋求牙科治療的患者比例仍然高得驚人,超過 40%,儘管我們的研究缺乏這類信息。此外,先前研究中報告的幾乎三分之二的患者在入院前已經由他們的牙醫或初級保健醫生口服給予抗生素,這個數字從 57%增加到 63%。人們認為,過度依賴抗生素而不是尋求治療根本原因,會導致次優的患者護理。因此,需要預測評分和算法來確定有風險的患者。
4.2. Limitations of the Study
4. 2. 研究的局限性
Our research has some important limitations and restrictions. To begin, the study was a single-center investigation of patients who had been admitted to the medical facility for odontogenic infections. Second, because of the retrospective design, we had to rely on the data from medical records; as a result, statistical analysis was susceptible to the risk of being inaccurate due to human error. Additionally, the retrospective study design impacts our results, as the research depends on the accuracy of both patient information tracking and the digital transcription of data from paper records. Limited by the retrospective design of our study, we could not perform a dynamic profile analysis of CRP and NLR, which may offer more helpful information. Other limitations are represented by country-specific features, since all patients were from Romania, and the oral hygiene can influence the severity of odontogenic infections. To provide more evidence in support of our results, further prospective research should be carried out.
我們的研究有一些重要的局限性和限制。首先,該研究是對因牙源性感染而入住醫療機構的患者進行的單中心調查。其次,由於採用回顧性設計,我們不得不依賴醫療記錄中的數據;因此,統計分析容易因人為錯誤而產生不準確的風險。此外,回顧性研究設計會影響我們的結果,因為研究依賴於患者信息跟踪和從紙質記錄中數位轉錄數據的準確性。由於我們研究的回顧性設計的限制,我們無法對 CRP 和 NLR 進行動態概況分析,這可能會提供更有幫助的信息。其他限制因素是國家/地區的特定特徵,因為所有患者都來自羅馬尼亞,而且口腔衛生會影響牙源性感染的嚴重程度。為了提供更多證據來支持我們的結果,應進行進一步的前瞻性研究。
5. Conclusions 5. 結論
This research aimed to determine whether there is a significant correlation between increased levels of inflammatory serum markers, as measured by the NLR and CRP, and the severity of odontogenic infections, as measured by the Symptom Severity score. The connection between these markers was discovered as an accurate predictor of OI severity. Thus, it can be concluded that CRP-NLR is a reliable and inexpensive biomarker to provide the severity of odontogenic infections that can be incorporated into other prognostic models to help determine the severity of odontogenic infections. Medical practitioners and their dental teams should be instructed to use the NLR-CRP score for the early identification and prognosis of severe odontogenic infections, hence potentially improving disease treatment choices.
本研究旨在確定通過 NLR 和 CRP 測量的炎症血清標誌物水平升高與通過症狀嚴重程度評分測量的牙源性感染嚴重程度之間是否存在顯著相關性。 這些標誌物之間的聯繫被發現是 OI 嚴重程度的準確預測指標。 因此,可以得出結論,CRP-NLR 是一種可靠且廉價的生物標誌物,可以提供牙源性感染的嚴重程度,可以將其納入其他預後模型中,以幫助確定牙源性感染的嚴重程度。 應指導醫療從業人員及其牙科團隊使用 NLR-CRP 評分來早期識別和預測嚴重牙源性感染,從而可能改善疾病治療選擇。
Author Contributions 作者貢獻
Conceptualization: M.P.; methodology: M.P. software: S.U.; validation: O.A.; formal analysis: M.P.; investigation: S.T.; resources: S.T. and O.R.; data curation: O.A.; writing—original draft preparation: O.A. and H.U.; writing—review and editing: S.T. and V.B.; visualization: H.U. and V.B.; supervision: B.A.B. and V.B.; project administration: B.A.B. and O.R. All authors have read and agreed to the published version of the manuscript.
概念化:M.P.;方法學:M.P.;軟體:S.U.;驗證:O.A.;正式分析:M.P.;調查:S.T.;資源:S.T.和 O.R.;資料管理:O.A.;寫作—初稿準備:O.A.和 H.U.;寫作—審閱和編輯:S.T.和 V.B.;視覺化:H.U.和 V.B.;監督:B.A.B.和 V.B.;專案管理:B.A.B.和 O.R.。所有作者都已閱讀並同意已發布的版本。
Institutional Review Board Statement
機構審查委員會聲明
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Victor Babes, University of Medicine and Pharmacy in Timisoara, with the approval number I-27098 from 14 October 2022.
該研究根據赫爾辛基宣言的指導方針進行,並獲得蒂米什瓦拉醫藥大學 Victor Babes 倫理委員會的批准,批准號為 I-27098,日期為 2022 年 10 月 14 日。
Informed Consent Statement
知情同意聲明
Written informed consent has been obtained from the patients to publish this paper.
已獲得患者的書面知情同意,以發表本文。
Data Availability Statement
數據可用性聲明
Data available on request.
數據可應要求提供。
Conflicts of Interest 利益衝突
The authors declare no conflict of interest.
作者聲明沒有利益衝突。
Funding Statement 經費聲明
This research received no external funding.
本研究未獲得任何外部資金。
Footnotes 腳註
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
免責聲明/出版者聲明:所有出版物中包含的聲明、意見和數據僅為個別作者和貢獻者的觀點,不代表 MDPI 和/或編輯的觀點。 MDPI 和/或編輯不對因內容中提及的任何想法、方法、說明或產品而導致的人員或財產傷害承擔責任。
References 參考文獻
-
1.Alotaibi N., Cloutier L., Khaldoun E., Bois E., Chirat M., Salvan D. Criteria for admission of odontogenic infections at high risk of deep neck space infection. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2015;132:261–264. doi: 10.1016/j.anorl.2015.08.007. [DOI] [PubMed] [Google Scholar]
1. Alotaibi N.、Cloutier L.、Khaldoun E.、Bois E.、Chirat M.、Salvan D. 深頸部感染高風險的牙源性感染入院標準。 Eur. Ann. Otorhinolaryngol。頭頸部疾病。 2015;132:261–264。 doi: 10.1016/j.anorl.2015.08.007。 [DOI] [PubMed] [Google Scholar] -
2.Bali R.K., Sharma P., Gaba S., Kaur A., Ghanghas P. A review of complications of odontogenic infections. Natl. J. Maxillofac. Surg. 2015;6:136–143. doi: 10.4103/0975-5950.183867. [DOI] [PMC free article] [PubMed] [Google Scholar]
2. Bali R.K.、Sharma P.、Gaba S.、Kaur A.、Ghanghas P. 牙源性感染併發症的回顧。 Natl. J. Maxillofac。手術。 2015;6:136–143。 doi: 10.4103/0975-5950.183867。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
3.Blankson P.-K., Parkins G., Boamah M.O., Abdulai A.E., Ahmed A.-M., Bondorin S., Nuamah I. Severe odontogenic infections: A 5-year review of a major referral hospital in Ghana. Pan Afr. Med. J. 2019;32:71. doi: 10.11604/pamj.2019.32.71.17698. [DOI] [PMC free article] [PubMed] [Google Scholar]
3. Blankson P.-K.、Parkins G.、Boamah M.O.、Abdulai A.E.、Ahmed A.-M.、Bondorin S.、Nuamah I. 嚴重的牙源性感染:迦納一家主要轉診醫院的 5 年回顧。泛非醫學雜誌。 2019;32:71。 doi: 10.11604/pamj.2019.32.71.17698。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
4.Sánchez R., Mirada E., Arias J., Paño J.R., Burgueño Garcia M. Severe odontogenic infections: Epidemiological, microbiological and therapeutic factors. Med. Oral Patol. Oral Cirugía Bucal. 2011;16:670–676. doi: 10.4317/medoral.16995. [DOI] [PubMed] [Google Scholar]
4. Sánchez R.、Mirada E.、Arias J.、Paño J.R.、Burgueño Garcia M. 嚴重的牙源性感染:流行病學、微生物學和治療因素。 Med. Oral Patol。 Oral Cirugía Bucal。 2011;16:670–676。 doi: 10.4317/medoral.16995。 [DOI] [PubMed] [Google Scholar] -
5.Stephens M.B., Wiedemer J.P., Kushner G.M. Dental Problems in Primary Care. Am. Fam. Physician. 2018;98:654–660. [PubMed] [Google Scholar]
5.Stephens M.B.、Wiedemer J.P.、Kushner G.M. 初級保健中的牙科問題。 美國家庭醫生。 2018;98:654–660。 [PubMed] [Google Scholar] -
6.Ince N., Güçlü E., Sungur M.A., Karabay O. Evaluation of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio in patients with cellulitis. Rev. Assoc. Med. Bras. 2020;66:1077–1081. doi: 10.1590/1806-9282.66.8.1077. [DOI] [PubMed] [Google Scholar]
6.Ince N.、Güçlü E.、Sungur M.A.、Karabay O. 評估蜂窩性組織炎患者的中性粒細胞與淋巴細胞比率、血小板與淋巴細胞比率以及淋巴細胞與單核細胞比率。 Rev. Assoc. Med. Bras。 2020;66:1077–1081。 doi: 10.1590/1806-9282.66.8.1077。 [DOI] [PubMed] [Google Scholar] -
7.Shumilah A.M., Othman A.M., Al-Madhagi A.K. Accuracy of neutrophil to lymphocyte and monocyte to lymphocyte ratios as new inflammatory markers in acute coronary syndrome. BMC Cardiovasc. Disord. 2021;21:422. doi: 10.1186/s12872-021-02236-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
7.Shumilah A.M.、Othman A.M.、Al-Madhagi A.K. 中性粒細胞與淋巴細胞比率和單核細胞與淋巴細胞比率作為急性冠狀動脈綜合徵的新炎症標誌物的準確性。 BMC 心血管疾病。 2021;21:422。 doi: 10.1186/s12872-021-02236-7。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
8.Spoto S., Lupoi D.M., Valeriani E., Fogolari M., Locorriere L., Anguissola G.B., Battifoglia G., Caputo D., Coppola A., Costantino S., et al. Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit. Medicina. 2021;57:811. doi: 10.3390/medicina57080811. [DOI] [PMC free article] [PubMed] [Google Scholar]
8.Spoto S.、Lupoi D.M.、Valeriani E.、Fogolari M.、Locorriere L.、Anguissola G.B.、Battifoglia G.、Caputo D.、Coppola A.、Costantino S. 等人。 重症監護室外敗血症患者中性粒細胞與淋巴細胞比率和血小板與淋巴細胞比率的診斷準確性和預後價值。 醫學。 2021;57:811。 doi: 10.3390/medicina57080811。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
9.Gurgus D., Grigoras M.L., Motoc A.G.M., Zamfir C.L., Cornianu M., Faur C.I., Pop D.L., Folescu R. Clinical relevance and accuracy of p63 and TTF-1 for better approach of small cell lung carcinoma versus poorly differentiated nonkeratinizing squamous cell carcinoma. Rom. J. Morphol. Embryol. 2019;60:139–143. [PubMed] [Google Scholar]
9. Gurgus D.、Grigoras M.L.、Motoc A.G.M.、Zamfir C.L.、Cornianu M.、Faur C.I.、Pop D.L.、Folescu R. p63 和 TTF-1 在更好地區分小細胞肺癌與低分化非角化鱗狀細胞癌的臨床相關性和準確性。Rom. J. Morphol. Embryol. 2019;60:139–143。 [PubMed] [Google Scholar] -
10.Bilgen Ö., Atici T., Durak K., Karaeminoğullari, Bilgen M.S. C-reactive Protein Values and Erythrocyte Sedimentation Rates after Total Hip and Total Knee Arthroplasty. J. Int. Med. Res. 2001;29:7–12. doi: 10.1177/147323000102900102. [DOI] [PubMed] [Google Scholar]
10. Bilgen Ö.、Atici T.、Durak K.、Karaeminoğullari、Bilgen M.S. 全髖關節和全膝關節置換術後 C 反應蛋白值和紅血球沉降率。J. Int. Med. Res. 2001;29:7–12。doi: 10.1177/147323000102900102。 [DOI] [PubMed] [Google Scholar] -
11.Jundt J.S., Gutta R. Characteristics and cost impact of severe odontogenic infections. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012;114:558–566. doi: 10.1016/j.oooo.2011.10.044. [DOI] [PubMed] [Google Scholar]
11. Jundt J.S.、Gutta R. 嚴重齒源性感染的特徵和成本影響。Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012;114:558–566。doi: 10.1016/j.oooo.2011.10.044。 [DOI] [PubMed] [Google Scholar] -
12.Sutter R., Tschudin-Sutter S., Grize L., Widmer A.F., Marsch S., Rüegg S. Acute phase proteins and white blood cell levels for prediction of infectious complications in status epilepticus. Crit. Care. 2011;15:R274. doi: 10.1186/cc10555. [DOI] [PMC free article] [PubMed] [Google Scholar]
12. Sutter R.、Tschudin-Sutter S.、Grize L.、Widmer A.F.、Marsch S.、Rüegg S. 急性期蛋白和白血球水平用於預測癲癇持續狀態下的感染併發症。Crit. Care. 2011;15:R274。doi: 10.1186/cc10555。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
13.Boucher N.E., Hanrahan J.J., Kihara F.Y. Occurrence of C-Reactive Protein in Oral Disease. J. Dent. Res. 1967;46:624. doi: 10.1177/00220345670460033001. [DOI] [PubMed] [Google Scholar]
13.Boucher N.E., Hanrahan J.J., Kihara F.Y. Occurrence of C-Reactive Protein in Oral Disease. J. Dent. Res. 1967;46:624. doi: 10.1177/00220345670460033001. [DOI] [PubMed] [Google Scholar] -
14.Heimdahl A., Nord C.E. Orofacial infections of odontogenic origin. Scand. J. Infect. Dis. 1983;39:86–91. [PubMed] [Google Scholar]
14. Heimdahl A., Nord C.E. 牙源性口面部感染。Scand. J. Infect. Dis. 1983;39:86–91。 [PubMed] [Google Scholar] -
15.Stathopoulos P., Igoumenakis D., Shuttleworth J., Smith W., Ameerally P. Predictive factors of hospital stay in patients with odontogenic maxillofacial infections: The role of C-reactive protein. Br. J. Oral Maxillofac. Surg. 2017;55:367–370. doi: 10.1016/j.bjoms.2016.11.004. [DOI] [PubMed] [Google Scholar]
15. Stathopoulos P., Igoumenakis D., Shuttleworth J., Smith W., Ameerally P. C-反应蛋白在预测牙源性颌面部感染患者住院时间中的作用。Br. J. Oral Maxillofac. Surg. 2017;55:367–370。doi: 10.1016/j.bjoms.2016.11.004。 [DOI] [PubMed] [Google Scholar] -
16.Ioan Faur C., Abu-Awwad A., Pop D.L., Zamfir C.L., Gurgus D., Hoinoiu T., Motoc A., Haivas C., Grigoraș M.L., Folescu R. Liquid Nitrogen Efficiency in Treatment of Giant Cell Tumor of Bone and Prevention of Recurrence. Appl. Sci. 2020;10:6310. doi: 10.3390/app10186310. [DOI] [Google Scholar]
16. Ioan Faur C., Abu-Awwad A., Pop D.L., Zamfir C.L., Gurgus D., Hoinoiu T., Motoc A., Haivas C., Grigoraș M.L., Folescu R. 液氮在治療骨巨細胞瘤和預防復發中的效率。Appl. Sci. 2020;10:6310。doi: 10.3390/app10186310。 [DOI] [Google Scholar] -
17.Pepys M.B., Hirschfield G.M. C-reactive protein: A critical update. J. Clin. Investig. 2003;111:1805–1812. doi: 10.1172/JCI200318921. [DOI] [PMC free article] [PubMed] [Google Scholar]
17.Pepys M.B., Hirschfield G.M. C 反應蛋白:重要更新。 J. Clin. Investig. 2003;111:1805–1812。 doi: 10.1172/JCI200318921。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
18.De Jager C.P., Van Wijk P.T., Mathoera R.B., De Jongh-Leuvenink J., Van Der Poll T., Wever P.C. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit. Care. 2010;14:R192. doi: 10.1186/cc9309. [DOI] [PMC free article] [PubMed] [Google Scholar]
18.De Jager C.P., Van Wijk P.T., Mathoera R.B., De Jongh-Leuvenink J., Van Der Poll T., Wever P.C. 急診科淋巴細胞減少症和中性粒細胞-淋巴細胞計數比率比傳統感染指標更好地預測菌血症。 Crit. Care. 2010;14:R192。 doi: 10.1186/cc9309。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
19.Lowsby R., Gomes C., Jarman I., Lisboa P., Nee P.A., Vardhan M., Eckersley T., Saleh R., Mills H. Neutrophil to lymphocyte count ratio as an early indicator of bloodstream infection in the emergency department. Emerg. Med. J. 2015;32:531–534. doi: 10.1136/emermed-2014-204071. [DOI] [PubMed] [Google Scholar]
19.Lowsby R., Gomes C., Jarman I., Lisboa P., Nee P.A., Vardhan M., Eckersley T., Saleh R., Mills H. 中性粒細胞與淋巴細胞計數比率作為急診科血流感染的早期指標。 Emerg. Med. J. 2015;32:531–534。 doi: 10.1136/emermed-2014-204071。 [DOI] [PubMed] [Google Scholar] -
20.Jiang J., Liu R., Yu X., Yang R., Xu H., Mao Z., Wang Y. The neutrophil-lymphocyte count ratio as a diagnostic marker for bacteremia: A systematic review and meta-analysis. Am. J. Emerg. Med. 2019;37:1482–1489. doi: 10.1016/j.ajem.2018.10.057. [DOI] [PubMed] [Google Scholar]
20.Jiang J., Liu R., Yu X., Yang R., Xu H., Mao Z., Wang Y. 中性粒細胞-淋巴細胞計數比率作為菌血症的診斷標記:系統回顧和薈萃分析。 Am. J. Emerg. Med. 2019;37:1482–1489。 doi: 10.1016/j.ajem.2018.10.057。 [DOI] [PubMed] [Google Scholar] -
21.Belei O., Ancusa O., Mara A., Olariu L., Amaricai E., Folescu R., Zamfir C.L., Gurgus D., Motoc A.G., Stanga L.C., et al. Current Paradigm of Hepatitis E Virus Among Pediatric and Adult Patients. Front. Pediatr. 2021;30:721918. doi: 10.3389/fped.2021.721918. [DOI] [PMC free article] [PubMed] [Google Scholar]
21. Belei O., Ancusa O., Mara A., Olariu L., Amaricai E., Folescu R., Zamfir C.L., Gurgus D., Motoc A.G., Stanga L.C. 等。 兒童和成人患者中戊型肝炎病毒的現行範例。 Front. Pediatr. 2021;30:721918。 doi: 10.3389/fped.2021.721918。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
22.Niu D., Huang Q., Yang F., Tian W., Li C., Ding L., Fang H.-C., Zhao Y. Serum biomarkers to differentiate Gram-negative, Gram-positive and fungal infection in febrile patients. J. Med. Microbiol. 2021;70:001360. doi: 10.1099/jmm.0.001360. [DOI] [PubMed] [Google Scholar]
22. Niu D., Huang Q., Yang F., Tian W., Li C., Ding L., Fang H.-C., Zhao Y. 血清生物標誌物用於區分發熱患者的革蘭氏陰性菌、革蘭氏陽性菌和真菌感染。 J. Med. Microbiol. 2021;70:001360。 doi: 10.1099/jmm.0.001360。 [DOI] [PubMed] [Google Scholar] -
23.Li W., Hou M., Ding Z., Liu X., Shao Y., Li X. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 2021;12:686983. doi: 10.3389/fneur.2021.686983. [DOI] [PMC free article] [PubMed] [Google Scholar]
23. Li W., Hou M., Ding Z., Liu X., Shao Y., Li X. 中性粒細胞與淋巴細胞比率在卒中中的預後價值:系統回顧和薈萃分析。 Front. Neurol. 2021;12:686983。 doi: 10.3389/fneur.2021.686983。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
24.Lee M.-J., Park S.-D., Kwon S.W., Woo S.-I., Lee M.-D., Shin S.-H., Kim D.-H., Kwan J., Park K.-S. Relation Between Neutrophil-to-Lymphocyte Ratio and Index of Microcirculatory Resistance in Patients With ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Am. J. Cardiol. 2016;118:1323–1328. doi: 10.1016/j.amjcard.2016.07.072. [DOI] [PubMed] [Google Scholar]
24. Lee M.-J., Park S.-D., Kwon S.W., Woo S.-I., Lee M.-D., Shin S.-H., Kim D.-H., Kwan J., Park K.-S. ST 段抬高型心肌梗塞患者接受直接經皮冠狀動脈介入治療時,中性粒細胞與淋巴細胞比率和微循環阻力指數之間的關係。 Am. J. Cardiol. 2016;118:1323–1328。 doi: 10.1016/j.amjcard.2016.07.072。 [DOI] [PubMed] [Google Scholar] -
25.Adamstein N.H., MacFadyen J.G., Rose L.M., Glynn R.J., Dey A.K., Libby P., Tabas I.A., Mehta N.N., Ridker P.M. The neutrophil–lymphocyte ratio and incident atherosclerotic events: Analyses from five contemporary randomized trials. Eur. Heart J. 2021;42:896–903. doi: 10.1093/eurheartj/ehaa1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
25.Adamstein N.H.、MacFadyen J.G.、Rose L.M.、Glynn R.J.、Dey A.K.、Libby P.、Tabas I.A.、Mehta N.N.、Ridker P.M. The neutrophil–lymphocyte ratio and incident atherosclerotic events: Analyses from five contemporary randomized trials. Eur. Heart J. 2021;42:896–903. doi: 10.1093/eurheartj/ehaa1034. [DOI] [PMC free article] [PubMed] [Google Scholar] -
26.Park J.M. Neutrophil-to-lymphocyte ratio in trauma patients. J. Trauma Acute Care Surg. 2017;82:225–226. doi: 10.1097/TA.0000000000001266. [DOI] [PubMed] [Google Scholar]
26.Park J.M. Neutrophil-to-lymphocyte ratio in trauma patients. J. Trauma Acute Care Surg. 2017;82:225–226. doi: 10.1097/TA.0000000000001266. [DOI] [PubMed] [Google Scholar] -
27.Lee P.Y., Oen K.Q.X., Lim G.R.S., Hartono J.L., Muthiah M., Huang D.Q., Teo F.S.W., Li A.Y., Mak A., Chandran N.S., et al. Neutrophil-to-Lymphocyte Ratio Predicts Development of Immune-Related Adverse Events and Outcomes from Immune Checkpoint Blockade: A Case-Control Study. Cancers. 2021;13:1308. doi: 10.3390/cancers13061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
27.Lee P.Y.、Oen K.Q.X.、Lim G.R.S.、Hartono J.L.、Muthiah M.、Huang D.Q.、Teo F.S.W.、Li A.Y.、Mak A.、Chandran N.S.等。中性粒细胞与淋巴细胞比率预测免疫相关不良事件的发生以及免疫检查点阻断的预后:一项病例对照研究。《癌症》。2021;13:1308。doi: 10.3390/cancers13061308。[DOI] [PMC 免费文章] [PubMed] [Google Scholar] -
28.Fest J., Ruiter T.R., Koerkamp B.G., Rizopoulos D., Ikram M.A., Van Eijck C.H.J., Stricker B.H. The neutrophil-to-lymphocyte ratio is associated with mortality in the general population: The Rotterdam Study. Eur. J. Epidemiol. 2019;34:463–470. doi: 10.1007/s10654-018-0472-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
28.Fest J.、Ruiter T.R.、Koerkamp B.G.、Rizopoulos D.、Ikram M.A.、Van Eijck C.H.J.、Stricker B.H.。中性粒细胞与淋巴细胞比率与一般人群的死亡率相关:鹿特丹研究。《欧洲流行病学杂志》。2019;34:463–470。doi: 10.1007/s10654-018-0472-y。[DOI] [PMC 免费文章] [PubMed] [Google Scholar] -
29.Miloro M., Ghali G.E., Larsen P., Waite P. Peterson’s Principles of Oral and Maxillofacial Surgery. 3rd ed. People’s Medical Publishing House; Shelton, CT, USA: 2012. pp. 841–861. [Google Scholar]
29.Miloro M.、Ghali G.E.、Larsen P.、Waite P.。彼得森口腔颌面外科原理。第三版。人民卫生出版社;谢尔顿,康涅狄格州,美国:2012 年。第 841–861 页。[Google Scholar] -
30.Sainuddin S., Hague R., Howson K., Clark S. New admission scoring criteria for patients with odontogenic infections: A pilot study. J. Oral Maxilloc. Surg. 2016;55:86–89. doi: 10.1016/j.bjoms.2016.05.003. [DOI] [PubMed] [Google Scholar]
30.Sainuddin S.、Hague R.、Howson K.、Clark S.。牙源性感染患者新的入院评分标准:一项初步研究。《口腔颌面外科杂志》。2016;55:86–89。doi: 10.1016/j.bjoms.2016.05.003。[DOI] [PubMed] [Google Scholar] -
31.Steindel S.J. International classification of diseases, 10th edition, clinical modification and procedure coding system: Descriptive overview of the next generation HIPAA code sets. J. Am. Med. Inform. Assoc. 2010;17:274–282. doi: 10.1136/jamia.2009.001230. [DOI] [PMC free article] [PubMed] [Google Scholar]
31.Steindel S.J. 國際疾病分類第十版,臨床修改和程序編碼系統:下一代 HIPAA 代碼集的描述性概述。J. Am. Med. Inform. Assoc. 2010;17:274–282。doi: 10.1136/jamia.2009.001230。[DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
32.Lambden S., Laterre P.F., Levy M.M., Francois B. The SOFA score—Development, utility and challenges of accurate assessment in clinical trials. Crit. Care. 2019;23:374. doi: 10.1186/s13054-019-2663-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
32.Lambden S., Laterre P.F., Levy M.M., Francois B. SOFA 評分—臨床試驗中準確評估的發展、效用和挑戰。Crit. Care. 2019;23:374。doi: 10.1186/s13054-019-2663-7。[DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
33.Seppänen L., Rautemaa R., Lindqvist C., Lauhio A., Richardson R. Changing clinical features of odontogenic maxillofacial infections. Clin. Oral Investig. 2010;14:459–465. doi: 10.1007/s00784-009-0281-5. [DOI] [PubMed] [Google Scholar]
33.Seppänen L., Rautemaa R., Lindqvist C., Lauhio A., Richardson R. 牙源性頜面部感染的臨床特徵變化。Clin. Oral Investig. 2010;14:459–465。doi: 10.1007/s00784-009-0281-5。[DOI] [PubMed] [Google Scholar] -
34.Burnham R., Bhandari R., Bridle C. Changes in admission rates for spreading odontogenic infection resulting from changes in government policy about the dental schedule and remunerations. Br. J. Oral Maxillofac. Surg. 2011;49:26–28. doi: 10.1016/j.bjoms.2009.10.033. [DOI] [PubMed] [Google Scholar]
34.Burnham R., Bhandari R., Bridle C. 由於政府關於牙科時間表和報酬政策的變化,擴散性牙源性感染的入院率發生了變化。Br. J. Oral Maxillofac. Surg. 2011;49:26–28。doi: 10.1016/j.bjoms.2009.10.033。[DOI] [PubMed] [Google Scholar] -
35.Edman-Wallér J., Ljungström L., Jacobsson G., Andersson R., Werner M. Systemic symptoms predict presence or development of severe sepsis and septic shock. Infect. Dis. 2015;48:209–214. doi: 10.3109/23744235.2015.1104719. [DOI] [PubMed] [Google Scholar]
35.Edman-Wallér J.、Ljungström L.、Jacobsson G.、Andersson R.、Werner M. 全身性症状預測嚴重敗血症和感染性休克的發生或發展。Infect. Dis. 2015;48:209–214。doi: 10.3109/23744235.2015.1104719。[DOI] [PubMed] [Google Scholar] -
36.Póvoa P., Coelho L., Almeida E., Fernandes A., Mealha R., Moreira P., Sabino H. Early identification of intensive care unit-acquired infections with daily monitoring of C-reactive protein: A prospective observational study. Crit. Care. 2006;10:R63. doi: 10.1186/cc4892. [DOI] [PMC free article] [PubMed] [Google Scholar]
36.Póvoa P.、Coelho L.、Almeida E.、Fernandes A.、Mealha R.、Moreira P.、Sabino H. 通過每日監測 C 反應蛋白早期識別重症監護病房獲得性感染:一項前瞻性觀察研究。Crit. Care. 2006;10:R63。doi: 10.1186/cc4892。[DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
37.Bagul R., Chandan S., Sane V.D., Patil S., Yadav D. Comparative Evaluation of C-Reactive Protein and WBC Count in Fascial Space Infections of Odontogenic Origin. J. Maxillofac. Oral Surg. 2016;16:238–242. doi: 10.1007/s12663-016-0953-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
37.Bagul R.、Chandan S.、Sane V.D.、Patil S.、Yadav D. C 反應蛋白和 WBC 計數在牙源性筋膜間隙感染中的比較評價。J. Maxillofac. Oral Surg. 2016;16:238–242。doi: 10.1007/s12663-016-0953-z。[DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
38.John C.R., Gandhi S., Singh I., James T.T. Efficacy of C-Reactive protein as a marker in patients with odontogenic fascial space infection: A prospective analytical study. J. NTR Univ. Health. Sci. 2021;10:76–81. [Google Scholar]
38.John C.R.、Gandhi S.、Singh I.、James T.T. C 反應蛋白作為牙源性筋膜間隙感染患者標誌物的功效:一項前瞻性分析研究。J. NTR Univ. Health. Sci. 2021;10:76–81。[Google Scholar] -
39.Barreto V.T., Isaac A., Bhimidi P., Nguyen C., Jones G. Trends of C-Reactive Protein Laboratory Values With White Blood Cell Count Levels in Maxillofacial Infections. J. Oral Maxillofac. Surg. 2013;71:31–32. doi: 10.1016/j.joms.2013.06.055. [DOI] [Google Scholar]
39. Barreto V.T.、Isaac A.、Bhimidi P.、Nguyen C.、Jones G. 上頜面感染中 C 反應蛋白實驗室數值與白血球計數水平的趨勢。口腔頜面外科雜誌。2013;71:31–32。doi: 10.1016/j.joms.2013.06.055。 [DOI] [Google Scholar] -
40.Huang Z., Fu Z., Huang W., Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg. Med. 2020;38:641–647. doi: 10.1016/j.ajem.2019.10.023. [DOI] [PubMed] [Google Scholar]
40. Huang Z.、Fu Z.、Huang W.、Huang K. 中性粒細胞與淋巴細胞比率在敗血症中的預後價值:一項統合分析。美國急診醫學雜誌。2020;38:641–647。doi: 10.1016/j.ajem.2019.10.023。 [DOI] [PubMed] [Google Scholar] -
41.Josse J.M., Cleghorn M.C., Ramji K.M., Jiang H., Elnahas A., Jackson T.D., Okrainec A., Quereshy F.A. The neutrophil/lymphocyte ratio predicts major perioperative complications in patients undergoing colorectal surgery. Color. Dis. 2016;18:236–242. doi: 10.1111/codi.13373. [DOI] [PubMed] [Google Scholar]
41. Josse J.M.、Cleghorn M.C.、Ramji K.M.、Jiang H.、Elnahas A.、Jackson T.D.、Okrainec A.、Quereshy F.A. 中性粒細胞/淋巴細胞比率可預測接受大腸直腸手術患者的主要圍手術期併發症。顏色。疾病。2016;18:236–242。doi: 10.1111/codi.13373。 [DOI] [PubMed] [Google Scholar] -
42.Silberman S., Abu-Yunis U., Tauber R., Shavit L., Grenader T., Fink D., Bitran D., Merin O. Neutrophil-Lymphocyte Ratio: Prognostic Impact in Heart Surgery. Early Outcomes and Late Survival. Ann. Thorac. Surg. 2018;105:581–586. doi: 10.1016/j.athoracsur.2017.07.033. [DOI] [PubMed] [Google Scholar]
42.Silberman S., Abu-Yunis U., Tauber R., Shavit L., Grenader T., Fink D., Bitran D., Merin O. Neutrophil-Lymphocyte Ratio: Prognostic Impact in Heart Surgery. Early Outcomes and Late Survival. Ann. Thorac. Surg. 2018;105:581–586. doi: 10.1016/j.athoracsur.2017.07.033. [DOI] [PubMed] [Google Scholar] -
43.Hajibandeh S., Hajibandeh S., Hobbs N., Mansour M. Neutrophil-to-lymphocyte ratio predicts acute appendicitis and distinguishes between complicated and uncomplicated appendicitis: A systematic review and meta-analysis. Am. J. Surg. 2020;219:154–163. doi: 10.1016/j.amjsurg.2019.04.018. [DOI] [PubMed] [Google Scholar]
43.Hajibandeh S., Hajibandeh S., Hobbs N., Mansour M. 嗜中性白血球與淋巴球比率預測急性闌尾炎,並區分複雜性與非複雜性闌尾炎:系統性回顧與統合分析。 Am. J. Surg. 2020;219:154–163。doi: 10.1016/j.amjsurg.2019.04.018。 [DOI] [PubMed] [Google Scholar] -
44.Gallagher N., Collyer J., Bowe C.M. Neutrophil to Lymphocyte Ratio as a Prognostic Marker of Deep Neck Space Infections Secondary to Odontogenic Infection. Br. J. Oral Maxillofac. Surg. 2021;59:228–232. doi: 10.1016/j.bjoms.2020.08.075. [DOI] [PubMed] [Google Scholar]
44.Gallagher N., Collyer J., Bowe C.M. 嗜中性白血球與淋巴球比率作為牙源性感染引起的深頸部空間感染的預後指標。 Br. J. Oral Maxillofac. Surg. 2021;59:228–232。doi: 10.1016/j.bjoms.2020.08.075。 [DOI] [PubMed] [Google Scholar] -
45.Russell C.D., Parajuli A., Gale H.J., Bulteel N.S., Schuetz P., de Jager C.P., Loonen A.J., Merekoulias G.I., Baillie J.K. The utility of peripheral blood leucocyte ratios as biomarkers in infectious diseases: A systematic review and meta-analysis. J. Infect. 2019;78:339–348. doi: 10.1016/j.jinf.2019.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
45.Russell C.D., Parajuli A., Gale H.J., Bulteel N.S., Schuetz P., de Jager C.P., Loonen A.J., Merekoulias G.I., Baillie J.K. 周邊血白血球比率作為傳染病生物標記的效用:系統性回顧與統合分析。 J. Infect. 2019;78:339–348。doi: 10.1016/j.jinf.2019.02.006。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
46.Vatankhah N., Jahangiri Y., Landry G.J., McLafferty R.B., Alkayed N.J., Moneta G.L., Azarbal A.F. Predictive value of neutrophil-to lymphocyte ratio in diabetic wound healing. J. Vasc. Surg. 2017;65:478–483. doi: 10.1016/j.jvs.2016.08.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
46.Vatankhah N., Jahangiri Y., Landry G.J., McLafferty R.B., Alkayed N.J., Moneta G.L., Azarbal A.F. 嗜中性白血球與淋巴球比率在糖尿病傷口癒合中的預測價值。 J. Vasc. Surg. 2017;65:478–483。doi: 10.1016/j.jvs.2016.08.108。 [DOI] [PMC 免費文章] [PubMed] [Google Scholar] -
47.Dogruel F., Gonen Z.-B., Gunay-Canpolat D., Zararsiz G., Alkan A. The Neutrophil-to-Lymphocyte ratio as a marker of recovery status in patients with severe dental infection. Med. Oral Patol. Oral Cir. Bucal. 2017;22:440–445. doi: 10.4317/medoral.21915. [DOI] [PMC free article] [PubMed] [Google Scholar]
47. Dogruel F., Gonen Z.-B., Gunay-Canpolat D., Zararsiz G., Alkan A. 中性粒细胞与淋巴细胞比率作为严重牙科感染患者恢复状态的标志物。Med. Oral Patol. Oral Cir. Bucal. 2017;22:440–445。doi: 10.4317/medoral.21915。 [DOI] [PMC 免费文章] [PubMed] [Google Scholar] -
48.Fu B., McGowan K., Sun J.H., Batstone M. Increasing frequency and severity of odontogenic infection requiring hospital admission and surgical management. Br. J. Oral Maxillofac. Surg. 2020;58:409–415. doi: 10.1016/j.bjoms.2020.01.011. [DOI] [PubMed] [Google Scholar]
48. Fu B., McGowan K., Sun J.H., Batstone M. 需要住院和手术治疗的牙源性感染的频率和严重程度不断增加。Br. J. Oral Maxillofac. Surg. 2020;58:409–415。doi: 10.1016/j.bjoms.2020.01.011。 [DOI] [PubMed] [Google Scholar]
Associated Data 相关数据
This section collects any data citations, data availability statements, or supplementary materials included in this article.
本节收集本文中包含的任何数据引用、数据可用性声明或补充材料。
Data Availability Statement
數據可用性聲明
Data available on request.
數據可應要求提供。